Neorickettsia risticii
| Neorickettsia risticii | |
|---|---|

| |
| Neorickettsia risticii phylogenetic tree based on 16S rRNA gene sequences | |
| Scientific classification | |
| Domain: | |
| Phylum: | |
| Class: | |
| Order: | |
| Family: | |
| Genus: | |
| Species: | N. risticii
|
| Binomial name | |
| Neorickettsia risticii (Dumler et al., 2001)
| |
| Synonyms | |
|
Ehrlichia risticii | |
Neorickettsia risticii, formerly Ehrlichia risticii, is an obligate intracellular gram-negative bacterium that typically lives as an endosymbiont in parasitic flatworms, specifically flukes.[1] N. risticii is the known causative agent of equine neorickettsiosis (also known as Potomac horse fever or PHF),[2] which gets its name from its discovery near the Potomac River in Maryland and Virginia.[3] N. risticii was first recovered from horses in this region in 1984 but was not recognized as the causative agent of PHF until 1979.[3] Potomac horse fever is currently endemic in the United States but has also been reported with lower frequency in other regions, including Canada, Brazil, Uruguay, and Europe.[4] PHF is a condition that is clinically important for horses since it can cause serious signs such as fever, diarrhea, colic, and laminitis.[5] PHF has a fatality rate of approximately 30%, making this condition a concern for horse owners in endemic regions.[5] N. risticii is typically acquired in the middle to late summer near freshwater streams or rivers, as well as on irrigated pastures.[6] This is a seasonal infection because it relies on the ingestion of an arthropod vector, which is more commonly found on pasture in the summer months.[7] Although N. risticii is a well known causative agent for PHF in horses, it may act as a potential pathogen in cats and dogs as well.[8] Not only has N. risticii been successfully cultured from monocytes of dogs and cats,[6] but cats have become clinically ill after experimental infection with the bacteria.[9] In addition, N. risticii has been isolated and cultured from human histiocytic lymphoma cells.[6]
Taxonomy, morphology, and identification
[edit]Neorickettsia risticii is a member of the order Rickettsiales and family Anaplasmataceae within the class Alphaproteobacteria.[10] N. risticii are obligate intracellular organisms[10] of equine monocytes/macrophages and glandular intestinal epithelium.[6] Individual organisms are small, pleomorphic (coccoid to ellipsoidal) gram negative aerobes that lack LPS and peptidoglycan in their cell walls.[11][12] They have two cell forms: a reticular body type form that is large and light, and a smaller elementary body type form that is electron-dense.[6][12][10] They can exist as individual cells or as morulae (colonies similar in appearance to mulberries) and replicate in parasitophorous vacuoles via binary fission within the host cell.[12][10] Identification can be done based on cell culture isolation, serology, or PCR assay.[1][6][13] However, N. risticii is rarely identified in monocytes from peripheral blood smears.[6] PCR assays can be performed on blood and feces (antemortem identification) or on fresh or formalin fixed tissues (postmortem identification).[6] N. risticii can be viewed using light microscopy with a variety of stains: Giemsa and Romanowsky stains will mark the bacteria dark blue to purple,[12] Machiavello will stain red, and hematoxylin eosin (H&E) will stain pale blue.[6]
Transmission
[edit]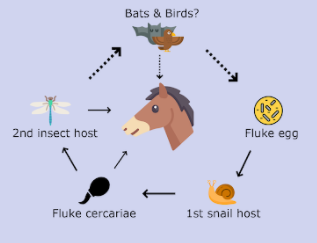
The exact mode of transmission of N. risticii has been undetermined for many years due to its complex life cycle. N. risticii is transmitted vertically inside a trematode (fluke), Acanthatrium oregonense, and the transmission of N. risticii is closely related to the life cycle of the fluke.[14][15] As the fluke develops and gets into the next host, N. risticii is passed on to the next host along with it.[15] The proposed mode of transmission involves two intermediate hosts (an aquatic snail and an aquatic insect such as caddisflies and mayflies).[14] The egg of the fluke is ingested by an aquatic snail. Then, the cercaria form of the fluke develops and emerges from the snail into the environment.[14] The cercaria then invades the second intermediate host, the larval or nymph stage of an aquatic insect. The cercaria develops into a metacercaria as the insect develops into an adult.[14] The adult insect is then ingested by an insectivore such as a bat or a swallow.[14][15] It is thought that bats and swallows serve as the definitive hosts for the fluke and natural reservoirs of N. risticii.[14]
It is proposed that horses can be exposed to N. risticii through two routes. Horses can be exposed through skin penetration by infected cercaria form of the fluke. This is commonly seen when horses are grazing near contaminated water sources.[16] Another route of exposure is through directly ingesting the second intermediate host, aquatic insects, containing the infected metacercariae.[14]
Pathogenesis
[edit]It is proposed that N. risticii is an obligate intracellular bacterium which prefer replicating in monocytes of the host.[17] Once phagocytized by the monocyte, the pathogen prevents lysosomal fusion with the phagosome thus escaping the host defense mechanism.[14] Once N. risticii establishes infection inside the host, the primary targets are the epithelial cells, mast cells, and macrophages located in the host's large intestine.[14] The infected intestinal epithelial cells suffer from impaired electrolyte transport and loss of microvilli, which contribute to decreased electrolyte absorption and increased water loss in the large intestine.[18] Therefore, diarrhea is one of the common clinical signs of equine neorickettsiosis.
Clinical significance
[edit]Neorickettsia risticii is the infectious cause of equine neorickettsiosis, or the colloquially termed Potomac horse fever (PHF).[5] This disease is acquired when horses ingest a trematode host that is infected with the bacteria.[5] Because of the presence of the arthropod vector, it seems that this disease is of concern in the summer, when warmer weather permits these vectors to be present on pasture.[7] N. risticii is able to stay inside these trematodes through their development stages, and can also be transmitted to future generations through a transovarial transmission route.[11] Once infected, the horse is not contagious to other horses, as the infection must be spread by the intermediate host ingestion.[5]
This disease can cause horses to become feverish, experience liquid diarrhea, show a quiet demeanor and go off their food, which can lead to colic and laminitis.[5] Intestinal lesions previously seen with PHF include pronounced enterocolitis with ulcerative erosions and evident reduction in villus projections.[19] The lesions will result in the horse having severe gastrointestinal disease, and reduced ability to absorb nutrients. Lesions that were linked to the presence of the bacteria in the blood include hepatitis, kidney tubule inflammation, loss of renal arterial blood supply, and inflammation of the adrenal glands.[19] There are also changes to the blood in response to infection, and early PHF can result in reduced white blood cells, including low neutrophils and low lymphocytes, while progression of PHF can result in an inflammatory response and increased white blood cells.[19] Replication of N. risticii happens within the epithelial lining of the intestines, and within myeloid cells such as macrophages, monocytes, and mast cells.[11] The condition can be fatal in 3 out of 10 horses that are infected, but up to one-third of horses infected have been shown to be asymptomatic, so there is variability in the disease presentation.[5] Due to the severe symptoms associated with the disease, and fatality rate, this condition is of concern for horse owners.
If a pregnant mare is infected with N. risticii and has symptoms of PHF, there is a chance that it may cause abortion and lesions in the fetus. Studies have been done on mares that were infected either naturally or artificially with N. risticii and experienced abortion. The fetuses had lesions of liver inflammation, heart inflammation, enterocolitis, and inflammation of the mesenteric lymph nodes.[20] Abortion seems to be a notable complication of PHF, as was showcased in a study that infected pregnant mares with N. risticii resulting in abortion in just over half of the subjects.[20] This infection does not cause inflammation of the placenta, and lesions are generally absent from the placenta or very minor, yet it does cause lesions in the fetus itself, which is quite unique.[20] PHF is not a well documented cause for equine abortion, and is often not chosen as a differential diagnosis.[20] However, it could be argued that N. risticii requires more research in this area, and could be a more common cause of equine abortion than was previously thought.
Diagnostics
[edit]Diagnosis of Potomac horse fever (PHF) is most commonly based on serological techniques and therefore requires collecting a blood sample from an infected horse. Neorickettsia risticii is detected in the blood using an indirect immunofluorescent antibody (IFA) test or by PCR identification.[21] The IFA serological test detects the presence of IgG and IgM antibodies against N. risticii in the blood, however does not differentiate whether an animal is actively infected or has had previous exposure.[22] The use of IFA at a single point in time does not provide an accurate diagnosis and therefore requires IFA testing at multiple time points to detect increasing antibody titres. Increasing antibody titres in conjunction with clinical signs is suggestive of an active PHF infection.[22] PCR assays can be performed on both the blood and stool of an infected animal and allows the detection of N. risticii in these samples.[4] PCR is the test of choice in vaccinated animals because these animals will have antibodies against N. risticii, which interferes with the IFA test.[22]
Cell culture isolation can also be used for the detection and isolation of Neorickettsia risticii, although it is a more time-consuming technique that requires specialized equipment and is not routinely used as a diagnostic method.[1] N. risticii is an obligate intracellular microorganism and as such is more technically difficult to culture, isolate, and ship to a diagnostic laboratory.[4] Cell culture isolation detects the presence of live bacteria and can be used to isolate bacteria from an infected animal, the environment, or a parasitic host.[1] Strain variation among isolates can be determined by identifying surface antigens or by performing whole-genome sequencing.[4] Molecular analysis surface antigens has found significant genetic and phenotypic variation in strains of N. risticii, these variations may contribute to vaccination failures.[23]
Treatment and prevention
[edit]The main clinical presentation of Neorickettsia risticii is Potomac horse fever (PHF). Timely diagnosis and treatment of PHF is important for preventing the disease from progressing and causing clinical signs such as laminitis, endotoxemia and colic. Successfully preventing this progression can greatly increase an infected horse's chance of survival.[24] Treatment of PHF utilizes a combination of antimicrobial and supportive therapy.[25] Oxytetracycline has been found to be the most successful antimicrobial treatment for PHF and has been correlated to increased survival time.[24] When treatment is delayed until after the onset of clinical signs, additional therapy with doxycycline, demeclocycline or rifampin has been associated with higher antibody titer levels than those of untreated animals.[26] In addition to antimicrobial treatment, supportive therapy for pain management, dehydration and gastrointestinal function should also be utilized to treat laminitis, endotoxemia and colic, respectively. Laminitis can be treated with a combination of cryotherapy and an opioid, such as butorphanol or morphine.[27] Intravenous lactated Ringer's solution can be given for fluid and electrolyte replenishment and Flunixin Meglumine can be used to treat signs of colic, both of which can help offset signs of endotoxemia and prevent endotoxic shock.[4]
There are currently two types of vaccines for Potomac horse fever available. One is an inactive monovalent vaccine that protects against PHF only, and the other is an inactive multivalent vaccine that is combined with a rabies vaccination. There is some evidence to show that the multivalent PHF/rabies vaccine provides lower immunogenicity in contrast to the monovalent PHF vaccine when it is given with a separate rabies vaccine.[28] The efficacy of these vaccines has been reported to be quite poor due to the fact that they contain only one of several strains of N. risticii, but studies have also shown that vaccinated horses that do become infected tend to show less severe clinical signs when compared to unvaccinated horses.[29] The vaccines are recommended to be given annually, but horses in endemic regions can be given a second dose three to four weeks following the initial vaccine to help increase the effectiveness. Pregnant mares should also be given an additional vaccine four to six weeks prior to foaling.[30]
See also
[edit]References
[edit]- ^ a b c d Teymournejad O, Lin M, Bekebrede H, Kamr A, Toribio RE, Arroyo LG, et al. (February 2020). "Neorickettsia Species That Causes Potomac Horse Fever". mBio. 11 (1) (published 25 February 2020). doi:10.1128/mBio.03429-19. ISSN 2150-7511. PMC 7042704. PMID 32098825. Wikidata Q89881646. (erratum)
- ^ Gibson KE, Rikihisa Y, Zhang C, Martin C (February 2005). "Neorickettsia risticii is vertically transmitted in the trematode Acanthatrium oregonense and horizontally transmitted to bats". Environmental Microbiology. 7 (2): 203–12. Bibcode:2005EnvMi...7..203G. doi:10.1111/j.1462-2920.2004.00683.x. PMID 15658987.
- ^ a b Chaichanasiriwithaya W, Rikihisa Y, Yamamoto S, Reed S, Crawford TB, Perryman LE, Palmer GH (December 1994). "Antigenic, morphologic, and molecular characterization of new Ehrlichia risticii isolates". Journal of Clinical Microbiology. 32 (12): 3026–33. doi:10.1128/JCM.32.12.3026-3033.1994. PMC 264219. PMID 7533780.
- ^ a b c d e Xiong Q, Bekebrede H, Sharma P, Arroyo LG, Baird JD, Rikihisa Y (October 2016). Dozois CM (ed.). "An Ecotype of Neorickettsia risticii Causing Potomac Horse Fever in Canada". Applied and Environmental Microbiology. 82 (19): 6030–6. Bibcode:2016ApEnM..82.6030X. doi:10.1128/AEM.01366-16. PMC 5038023. PMID 27474720.
- ^ a b c d e f g Roier, Erica C.R.; Costa, Renata L.; Pires, Marcus S.; Vilela, Joice A.R.; Santos, Tiago M. dos; Santos, Huarrisson A.; Baldani, Cristiane D.; Massard, Carlos L. (October 2016). "Epidemiological survey of Neorickettsia risticii in equids from the State of Rio de Janeiro, Brazil". Pesquisa Veterinária Brasileira. 36 (10): 939–946. doi:10.1590/S0100-736X2016001000004.
- ^ a b c d e f g h i Pusterla N, Madigan JE (2014). "Neorickettsia risticii". Equine Infectious Diseases. Elsevier. pp. 347–351.e2. doi:10.1016/b978-1-4557-0891-8.00040-3. ISBN 978-1-4557-0891-8.
- ^ a b McLaughlin B, Gough J (June 1996). "Potomac horse fever in southwestern Ontario". The Canadian Veterinary Journal. 37 (6): 367–8. PMC 1576412. PMID 8689598.
- ^ Ayllón T, Diniz PP, Breitschwerdt EB, Villaescusa A, Rodríguez-Franco F, Sainz A (February 2012). "Vector-borne diseases in client-owned and stray cats from Madrid, Spain". Vector Borne and Zoonotic Diseases. 12 (2): 143–50. doi:10.1089/vbz.2011.0729. PMID 22022820.
- ^ Lappin MR, Griffin B, Brunt J, Riley A, Burney D, Hawley J, et al. (April 2006). "Prevalence of Bartonella species, haemoplasma species, Ehrlichia species, Anaplasma phagocytophilum, and Neorickettsia risticii DNA in the blood of cats and their fleas in the United States". Journal of Feline Medicine and Surgery. 8 (2): 85–90. doi:10.1016/j.jfms.2005.08.003. PMC 10832684. PMID 16290092. S2CID 19187668.
- ^ a b c d Yu XJ, Walker DH (2006). "The Order Rickettsiales". In Dworkin M, Falkow S, Rosenberg E, Schleifer KH (eds.). The Prokaryotes. New York, NY: Springer New York. pp. 493–528. doi:10.1007/0-387-30745-1_20. ISBN 978-0-387-25495-1.
- ^ a b c Lin M, Zhang C, Gibson K, Rikihisa Y (October 2009). "Analysis of complete genome sequence of Neorickettsia risticii: causative agent of Potomac horse fever". Nucleic Acids Research. 37 (18): 6076–91. doi:10.1093/nar/gkp642. PMC 2764437. PMID 19661282.
- ^ a b c d Rikihisa Y (October 2006). "New findings on members of the family Anaplasmataceae of veterinary importance". Annals of the New York Academy of Sciences. 1078 (1): 438–45. Bibcode:2006NYASA1078..438R. doi:10.1196/annals.1374.083. PMID 17114752. S2CID 21179916.
- ^ Lappin MR, Griffin B, Brunt J, Riley A, Burney D, Hawley J, et al. (April 2006). "Prevalence of Bartonella species, haemoplasma species, Ehrlichia species, Anaplasma phagocytophilum, and Neorickettsia risticii DNA in the blood of cats and their fleas in the United States". Journal of Feline Medicine and Surgery. 8 (2): 85–90. doi:10.1016/j.jfms.2005.08.003. PMC 10832684. PMID 16290092. S2CID 19187668.
- ^ a b c d e f g h i Sellon DC, Long MT (2014). "Acknowledgments". Equine Infectious Diseases. Elsevier. pp. xi. doi:10.1016/b978-1-4557-0891-8.00078-6. ISBN 978-1-4557-0891-8.
- ^ a b c Madigan JE, Pusterla N, Johnson E, Chae JS, Pusterla JB, Derock E, Lawler SP (July 2000). "Transmission of Ehrlichia risticii, the agent of Potomac horse fever, using naturally infected aquatic insects and helminth vectors: preliminary report". Equine Veterinary Journal. 32 (4): 275–9. doi:10.2746/042516400777032219. PMID 10952374.
- ^ "Potomac Horse Fever: A Water-borne Equestrian Worry". Horse Canada. 16 January 2015. Retrieved 2020-11-15.
- ^ "Potomac Horse Fever - Digestive System". Merck Veterinary Manual. Retrieved 2020-11-15.
- ^ Rikihisa Y, Johnson GC, Wang YZ, Reed SM, Fertel R, Cooke HJ (May 1992). "Loss of absorptive capacity for sodium and chloride in the colon causes diarrhoea in Potomac horse fever". Research in Veterinary Science. 52 (3): 353–362. doi:10.1016/0034-5288(92)90037-3. PMID 1352409.
- ^ a b c Heller MC, McClure J, Pusterla N, Pusterla JB, Stahel S (May 2004). "Two cases of Neorickettsia (Ehrlichia) risticii infection in horses from Nova Scotia". The Canadian Veterinary Journal. 45 (5): 421–3. PMC 548627. PMID 15206592.
- ^ a b c d Coffman EA, Abd-Eldaim M, Craig LE (November 2008). "Abortion in a horse following Neorickettsia risticii infection". Journal of Veterinary Diagnostic Investigation. 20 (6): 827–30. doi:10.1177/104063870802000622. PMID 18987240. S2CID 3208314.
- ^ Gibson KE, Pastenkos G, Moesta S, Rikihisa Y (June 2011). "Neorickettsia risticii surface-exposed proteins: proteomics identification, recognition by naturally-infected horses, and strain variations". Veterinary Research. 42 (1): 71. doi:10.1186/1297-9716-42-71. PMC 3127766. PMID 21635728.
- ^ a b c Mott J, Rikihisa Y, Zhang Y, Reed SM, Yu CY (September 1997). "Comparison of PCR and culture to the indirect fluorescent-antibody test for diagnosis of Potomac horse fever". Journal of Clinical Microbiology. 35 (9): 2215–9. doi:10.1128/JCM.35.9.2215-2219.1997. PMC 229942. PMID 9276390.
- ^ Biswas B, Vemulapalli R, Dutta SK (August 1998). "Molecular basis for antigenic variation of a protective strain-specific antigen of Ehrlichia risticii". Infection and Immunity. 66 (8): 3682–8. doi:10.1128/IAI.66.8.3682-3688.1998. PMC 108402. PMID 9673249.
- ^ a b Bertin FR, Reising A, Slovis NM, Constable PD, Taylor SD (2013). "Clinical and clinicopathological factors associated with survival in 44 horses with equine neorickettsiosis (Potomac horse Fever)". Journal of Veterinary Internal Medicine. 27 (6): 1528–34. doi:10.1111/jvim.12209. PMID 24118378.
- ^ "Potomac Horse Fever - Digestive System". Merck Veterinary Manual. Retrieved 2020-11-10.
- ^ Rikihisa Y, Jiang BM (March 1989). "Effect of antibiotics on clinical, pathologic and immunologic responses in murine Potomac horse fever: protective effects of doxycycline". Veterinary Microbiology. 19 (3): 253–62. doi:10.1016/0378-1135(89)90071-0. PMID 2497577.
- ^ Durán MC, Marqués FJ (March 2016). "Detection of Neorickettsia risticii, the agent of Potomac horse fever, in a Gypsy Vanner stallion from Manitoba". The Canadian Veterinary Journal. 57 (3): 293–5. PMC 4751770. PMID 26933267.
- ^ McKenzie HC, Funk RA, Trager L, Werre SR, Crisman M (November 2019). "Immunogenicity of Potomac horse fever vaccine when simultaneously co-administered with rabies vaccine in a multivalent vaccine or as two monovalent vaccines at separate sites". Equine Veterinary Journal. 51 (6): 774–778. doi:10.1111/evj.13096. PMC 6850380. PMID 30859618.
- ^ Dutta SK, Vemulapalli R, Biswas B (February 1998). "Association of deficiency in antibody response to vaccine and heterogeneity of Ehrlichia risticii strains with Potomac horse fever vaccine failure in horses". Journal of Clinical Microbiology. 36 (2): 506–12. doi:10.1128/JCM.36.2.506-512.1998. PMC 104568. PMID 9466767.
- ^ "Potomac Horse Fever | AAEP". aaep.org. Retrieved 2020-11-10.
