Hemoglobin-G
Origins
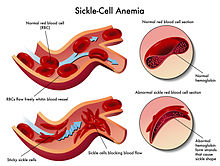
[edit]Hemoglobin G, Hemoglobin G-Philadelphia, or hbG, is a mutation of the cells that oxygenate blood. The G-Philadelphia variant is most commonly found in African Americans, with carriers being every 1 in 5,000.[1] The trait is normal-functioning and has no known negative effects.[2]
The mutation was first discovered in 1971, during the boom of research in to hemoglobin.[3] The push was backed by the desire to research the causes and possibly fight sickle cell anemia and other types of Anemia. Because the strict laws of clinical testing had not existed in the 1970s, clinical trials were conducted almost immediately upon the granting of the National Sickle Cell Act of 1971.[4]
Historical research
[edit]Schwartz et al confirmed that Hemoglobin G is a normal mutation of the combination of S and A alleles, which is reflected in the chart below.[2]
Recent findings
[edit]Over time the variant has been shown more commonly in people of African and of Asian descent.[citation needed] The clinical presentations of the gene mutation are regarded as either Microcytic or Hypochromic if they are detectable at all.[5] While the trait is not known to be abnormal on its own, the mutation of the gene can have an effect on the absorption of alcohol.[6] As well as physical difficulties with alcohol and other blood-altering substances, the hemoglobin has also been shown to effect the way the brain handles sleep disorders, like insomnia.[6] People with the G mutation are typically more likely to have issues oxygenating blood and because of this, Anemia was thought to be a side-effect of the mutation.[7]
The overall consensus among clinicians is that the "G-Philadelphia" mutation is harmless and has no clinical consequences.[8]
Clinical perspective
[edit]| Presumptive Diagnosis | Alpha Gene Arrangement | Functioning α-genes | Inheritance | Hgb G, % | Clinical Presentation | |
|---|---|---|---|---|---|---|
| uncomplicated G trait, no thalassemia | αG α/α α | 4 | Mediterranean | 20-25 | No defect | |
| alpha thal 2 with trans G trait | α -/αG – or – α/αG – | 2 | Mediterranean | 35-45 | Microcytic | |
| alpha thal 2 trait, G trait | α3.7G/α α | 3 | African American | 25-35 | Usually no defect | |
| alpha thal 2, G trait | α3.7G/- α | 2 | African plus other | 40-45 | Microcytic/Hypochromic | |
| alpha thal 2, homozygous G | α3.7G/α3.7G | 2 | African American | 95 | Microcytic/Hypochromic | |
| α thal 2/α thal 1, G trait (also known as H Disease, G trait) | α3.7G/ – – | 1 | rare | no A | Microcytic (MCV 55 fL) precipitation of beta-tetramers splenomegaly ineffective hematopoiesis bone marrow erythroid expansion |

References
[edit]- ^ a b "Anemia Associated with Hemoglobin G-Philadelphia". 2019-01-17.
- ^ a b Schwartz, H. C.; Spaet, T. H.; Zuelzer, W. W.; Neel, J. V.; Robinson, A. R.; Kaufman, S. F. (1 March 1957). "Combinations of Hemoglobin G, Hemoglobin S and Thalassemia Occurring in One Family". Blood. 12 (3): 238–250. CiteSeerX 10.1.1.830.2466. doi:10.1182/blood.V12.3.238.238. PMID 13403987.
- ^ Sancar, Gwendolyn B.; Tatsis, Basil; Cedeno, Marisol M.; Rieder, Ronald F. (1 November 1980). "Proportion of hemoglobin G Philadelphia (alpha 268 Asn leads to Lys beta 2) in heterozygotes is determined by alpha-globin gene deletions". Proceedings of the National Academy of Sciences. 77 (11): 6874–6878. doi:10.1073/pnas.77.11.6874. PMC 350393. PMID 6935689.
- ^ Winter, William P. (June 1990). "The Tertiary Diagnosis of Rare Hemoglobin Variants". Mayo Clinic Proceedings. 65 (6): 889–891. doi:10.1016/S0025-6196(12)62580-4. PMID 2195250.
- ^ Sheila, Dawling (17 January 2019). "Anemia Associated with Hemoglobin G-Philadelphia". Cancer Therapy Advisor.
- ^ a b Brower, Kirk J.; Aldrich, Michael S.; Robinson, Elizabeth A.R.; Zucker, Robert A.; Greden, John F. (March 2001). "Insomnia, Self-Medication, and Relapse to Alcoholism". American Journal of Psychiatry. 158 (3): 399–404. doi:10.1176/appi.ajp.158.3.399. PMC 3008542. PMID 11229980.
- ^ Rising, James A.; Sautter, Robert L.; Spicer, Serie J. (1 January 1974). "Hemoglobin G-Philadelphia/S: A Family Study of an Inherited Hybrid Hemoglobin". American Journal of Clinical Pathology. 61 (1): 92–102. doi:10.1093/ajcp/61.1.92.
- ^ "Hemoglobins – What the results mean". 2012-02-20.
