Food allergy
| Food allergy | |
|---|---|
 | |
| Hives on the back are a common allergy symptom. | |
| Specialty | Emergency medicine, allergy and immunology |
| Symptoms | Itchiness, swelling of the tongue, vomiting, diarrhea, hives, trouble breathing, low blood pressure[1] |
| Usual onset | Minutes to several hours of exposure[1] |
| Duration | Long term, some may resolve[2] |
| Causes | Immune response to food[1] |
| Risk factors | Family history, vitamin D deficiency, obesity, high levels of cleanliness[1][2] |
| Diagnostic method | Based on a medical history, elimination diet, skin prick test, oral food challenge[1][2] |
| Differential diagnosis | Food intolerance, celiac disease, food poisoning[1] |
| Prevention | Early exposure to potential allergens,[2][3] omalizumab |
| Treatment | Avoiding the food in question, having a plan if exposure occurs, medical alert jewelry[1][2] |
| Medication | Adrenaline (epinephrine)[1] |
| Frequency | ~6% (developed world)[1][2] |
A food allergy is an abnormal immune response to food. The symptoms of the allergic reaction may range from mild to severe. They may include itchiness, swelling of the tongue, vomiting, diarrhea, hives, trouble breathing, or low blood pressure. This typically occurs within minutes to several hours of exposure. When the symptoms are severe, it is known as anaphylaxis.[1] A food intolerance and food poisoning are separate conditions, not due to an immune response.[1][4]
Common foods involved include cow's milk, peanuts, eggs, shellfish, fish, tree nuts, soy, wheat, and sesame.[1][5][2][6] The common allergies vary depending on the country.[1] Risk factors include a family history of allergies, vitamin D deficiency, obesity, and high levels of cleanliness.[1][2] Allergies occur when immunoglobulin E (IgE), part of the body's immune system, binds to food molecules.[1] A protein in the food is usually the problem.[2] This triggers the release of inflammatory chemicals such as histamine.[1] Diagnosis is usually based on a medical history, elimination diet, skin prick test, blood tests for food-specific IgE antibodies, or oral food challenge.[1][2]
Management involves avoiding the food in question and having a plan if exposure occurs.[2] This plan may include giving adrenaline (epinephrine) and wearing medical alert jewelry.[1] Early childhood exposure to potential allergens may be protective against later development of a food allergy.[2][3] The benefits of allergen immunotherapy for treating food allergies are not proven, thus not recommended as of 2015[update].[7] Some types of food allergies among children resolve with age, including those to milk, eggs, and soy; while others such as to nuts and shellfish typically do not.[2]
In the developed world, about 4% to 8% of people have at least one food allergy.[1][2] They are more common in children than adults and appear to be increasing in frequency.[2] Male children appear to be more commonly affected than females.[2] Some allergies more commonly develop early in life, while others typically develop in later life.[1] In developed countries, more people believe they have food allergies when they actually do not have them.[8][9][10]
Signs and symptoms
[edit]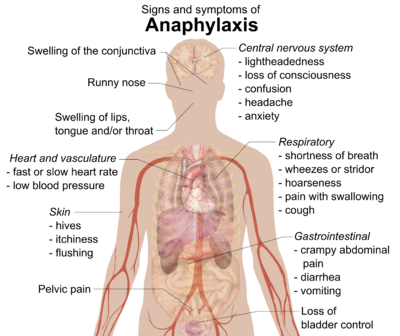
Food allergy symptoms occur within minutes to hours after exposure and may include:[11]
- Rash
- Hives[11]
- Itching of mouth, lips, tongue, throat, eyes, skin, or other areas[11]
- Swelling (angioedema) of lips, tongue, eyelids, or the whole face[11]
- Difficulty swallowing[11]
- Runny or congested nose[11]
- Hoarse voice[11]
- Wheezing and/or shortness of breath[11]
- Diarrhea, abdominal pain, and/or stomach cramps[11]
- Lightheadedness[11]
- Fainting[11]
- Nausea[11]
- Vomiting[11]
In some cases, however, onset of symptoms may be delayed for hours.[11]
Symptoms can vary. The amount of food needed to trigger a reaction also varies.[12]
Serious danger regarding allergies can begin when the respiratory tract or blood circulation is affected. The former can be indicated through wheezing and cyanosis. Poor blood circulation leads to a weak pulse, pale skin and fainting.[13]
A severe case of an allergic reaction, caused by symptoms affecting the respiratory tract and blood circulation, is called anaphylaxis. When symptoms are related to a drop in blood pressure, the person is said to be in anaphylactic shock. Anaphylaxis occurs when IgE antibodies are involved, and areas of the body that are not in direct contact with the food become affected and show symptoms.[14] Those with asthma or an allergy to peanuts, tree nuts, or seafood are at greater risk for anaphylaxis.
Causes
[edit]Common food allergies
[edit]Allergic reactions are abnormal immune responses that develop after exposure to a given food allergen.[15] Food allergens account for about 90% of all allergic reactions.[16] The most common food allergens include milk, eggs, peanuts, tree nuts, fish, shellfish, soy, and wheat,[17] which are referred to as "the big eight", and are required by US law to be on labels of foods that contain those foods.[18] In April 2021, President Biden signed the FASTER Act into law. This recognized sesame as the ninth US mandatory food label allergen.[19][20]
Peanuts, a member of the legume family, are one of the most common food allergens that induce reactions in both children and adults.[21] Affecting about 2% of the Western population, peanut allergies tend to cause more severe reactions and anaphylaxis than other food allergies.[22] Tree nuts, including almonds, brazil nuts, cashews, coconuts, hazelnuts, macadamia nuts, pecans, pistachios, pine nuts, and walnuts, are also common allergens. Affected individuals may be sensitive to one particular tree nut or many different ones.[23] Peanuts and seeds, including sesame seeds and poppy seeds, can be processed to extract oils, but trace amounts of protein may also elicit an allergic reaction.[23] Peanut and tree nut allergies are lifelong conditions for the majority of those affected, although evidence shows that ~20% of those with peanut allergies and 9% of those with tree nut allergies may outgrow them.[24]
Egg allergies affect about one in 50 children but are frequently outgrown when children reach age five.[25] Affected individuals can be sensitive to proteins both in the egg white and egg yolk, but most children are allergic to those in the white while most adults are allergic to those in the yolk.[26]
Cow's milk is the most common food allergen in infants and young children, yet many adults are also sensitized to cow's milk.[27] Many affected individuals cannot tolerate dairy products such as cheese and yogurt.[28] A small portion of children with milk allergy, roughly 10%, have a reaction to beef because it contains small amounts of protein that are also present in cow's milk.[29]
Shellfish, which are divided into crustaceans (shrimp, crab, lobster, etc.) and mollusks (mussel, oyster, scallop, squid, octopus, snail, etc.), are the most common food allergy in adults.[30] People may be allergic to other types of seafood, such as fish.[31] Fish allergies were found to be more common in countries that have high fish consumption compared to those with lower consumption.[32]
Other common food allergens include soy and wheat.[33] Those allergic to wheat may be sensitized to any protein in the wheat kernel.[34] To a lesser frequency, people may be mildly allergic to raw fruits and vegetables, a disease known as oral allergy syndrome.[33] Less common allergens include maize, spices, synthetic and natural colors,[35] and chemical additives.[36]
Balsam of Peru, which is in various foods, is in the "top five" allergens most commonly causing patch test reactions in people referred to dermatology clinics.[37]
Routes of exposure
[edit]Exposure to certain food proteins triggers the production of antigen-specific immunoglobulin E (IgE) antibodies, which, if unaccompanied by allergic symptoms, is known as allergic sensitization.[38] Oral ingestion is the main sensitization route for most food allergy cases, yet other routes of exposure include inhalation and skin contact.[39][34]
For example, inhaling airborne particles in a farm-scale or factory-scale peanut shelling/crushing environment, or from cooking, can induce respiratory effects in allergic individuals.[40] Furthermore, peanut allergies are much more common in adults who had oozing and crusted skin rashes as infants,[41] suggesting that impaired skin may be a risk factor for sensitization.[34][42] An estimated 28.5 million people worldwide are engaged in the seafood industry, which includes fishing, aquaculture, processing and industrial cooking.[43] In these occupational settings, individuals with fish and shellfish allergies are at high risk of exposure to allergenic proteins via aerosolization.[44][43] Respiratory symptoms may be induced by inhalation of wet aerosols from fresh fish handling, inhalation of dry aerosols from fishmeal processing, and dermal contact through skin breaks and cuts.[45][43] Another occupational food allergy that involves respiratory symptoms is "baker's asthma," which commonly develops in food service workers who work with baked goods.[46] Previous studies detected 40 allergens from wheat, some cross-reacted with rye proteins and a few cross-reacted with grass pollens.[47]
Allergic sensitization can occur via skin antigen exposure, which usually manifests as hives.[48] The skin has been suggested to be a critical sensitization route for peanut-allergic individuals.[49][40] Peanut allergies are much more common in adults who had oozing and crusted skin rashes as infants,[41] reinforcing that those with disrupted epithelial barriers, notably the skin barrier, are more prone to skin sensitization.[34] Environmental factors, such as exposure to food, microorganisms, creams, and detergents, may lead to skin barrier dysfunction.[50] Several studies reveal that children exposed to skin creams containing peanut oil are reported to have a higher risk of peanut allergy,[50] suggesting that impaired skin may be a risk factor for sensitization.[34][42]
Atopy
[edit]Food allergies develop more easily in people with the atopic syndrome, a very common combination of diseases: allergic rhinitis and conjunctivitis, eczema, and asthma.[51] The syndrome has a strong inherited component; a family history of allergic diseases can be indicative of the atopic syndrome.[medical citation needed]
Cross-reactivity
[edit]Some children who are allergic to cow's milk protein also show a cross-sensitivity to soy-based products.[52] Some infant formulas have their milk and soy proteins hydrolyzed, so when taken by infants, their immune systems do not recognize the allergen and they can safely consume the product. Hypoallergenic infant formulas can be based on proteins partially predigested to a less antigenic form. Other formulas, based on free amino acids, are the least antigenic and provide complete nutritional support in severe forms of milk allergy.[53]
Crustaceans (shrimp, crab, lobster, etc.) and molluscs (mussel, oyster, scallop, squid, octopus, snail, etc.) are different invertebrate classes, but the allergenic protein tropomyosin is present and responsible for cross-reactivity.[54]
People with latex allergy often also develop allergies to bananas, kiwifruit, avocados, and some other foods.[55]
Pathophysiology
[edit]
Conditions caused by food allergies are classified into three groups according to the mechanism of the allergic response:[56]
- IgE-mediated (classic) – the most common type, occurs shortly after eating and may involve anaphylaxis.
- Non-IgE mediated – characterized by an immune response not involving immunoglobulin E; may occur some hours after eating, complicating diagnosis
- IgE and/or non-IgE-mediated – a hybrid of the above two types
Allergic reactions are abnormal immune responses to certain substances that are normally harmless. When immune cells encounter the allergenic protein, IgE antibodies are produced; this is similar to the immune system's reaction to foreign pathogens. The IgE antibodies identify the allergenic proteins as harmful and initiate the allergic reaction. The harmful proteins are those that do not break down due to the strong bonds of the protein. IgE antibodies bind to a receptor on the surface of the protein, creating a tag, just as a virus or parasite becomes tagged. Why some proteins do not denature and subsequently trigger allergic reactions and hypersensitivity while others do is not entirely clear.[57]
Hypersensitivities are categorized according to the parts of the immune system that are attacked and the amount of time it takes for the response to occur. The four types of hypersensitivity reaction are: type 1, immediate IgE-mediated; type 2, cytotoxic; type 3, immune complex-mediated; and type 4, delayed cell-mediated.[58] The pathophysiology of allergic responses can be divided into two phases. The first is an acute response that occurs immediately after exposure to an allergen. This phase can either subside or progress into a "late-phase reaction" which can substantially prolong the symptoms of a response, and result in tissue damage.[citation needed]
Many food allergies are caused by hypersensitivities to particular proteins in different foods. Proteins have unique properties that allow them to become allergens, such as stabilizing forces in their tertiary and quaternary structures which prevent degradation during digestion. Many theoretically allergenic proteins cannot survive the destructive environment of the digestive tract, thus do not trigger hypersensitive reactions.[59]
Acute response
[edit]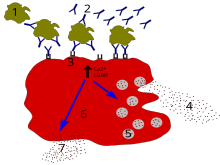
1 — antigen
2 — IgE antibody
3 — FcεRI receptor
4 — preformed mediators (histamine, proteases, chemokines, heparin)
5 — granules
6 — mast cell
7 — newly formed mediators (prostaglandins, leukotrienes, thromboxanes, PAF)
In the early stages of allergy, a type I hypersensitivity reaction against an allergen, encountered for the first time, causes a response in a type of immune cell called a TH2 lymphocyte, which belongs to a subset of T cells that produce a cytokine called interleukin-4 (IL-4). These TH2 cells interact with other lymphocytes called B cells, whose role is the production of antibodies. Coupled with signals provided by IL-4, this interaction stimulates the B cell to begin production of a large amount of a particular type of antibody known as IgE. Secreted IgE circulates in the blood and binds to an IgE-specific receptor (a kind of Fc receptor called FcεRI) on the surface of other kinds of immune cells called mast cells and basophils, which are both involved in the acute inflammatory response. The IgE-coated cells, at this stage, are sensitized to the allergen.[60]
If later exposure to the same allergen occurs, the allergen can bind to the IgE molecules held on the surface of the mast cells or basophils. Cross-linking of the IgE and Fc receptors occurs when more than one IgE-receptor complex interacts with the same allergenic molecule and activates the sensitized cell. Activated mast cells and basophils undergo a process called degranulation, during which they release histamine and other inflammatory chemical mediators (cytokines, interleukins, leukotrienes, and prostaglandins) from their granules into the surrounding tissue causing several systemic effects, such as vasodilation, mucous secretion, nerve stimulation, and smooth-muscle contraction. This results in rhinorrhea, itchiness, dyspnea, and anaphylaxis. Depending on the individual, the allergen, and the mode of introduction, the symptoms can be system-wide (classical anaphylaxis), or localized to particular body systems.[60]
Late-phase response
[edit]After the chemical mediators of the acute response subside, late-phase responses can often occur due to the migration of other leukocytes such as neutrophils, lymphocytes, eosinophils, and macrophages to the initial site. The reaction is usually seen 2–24 hours after the original reaction.[61] Cytokines from mast cells may also play a role in the persistence of long-term effects.[62]
Diagnosis
[edit]

Diagnosis is usually based on a medical history, elimination diet, skin prick test, blood tests for food-specific IgE antibodies, or oral food challenge.[1][2]
- For skin-prick tests, a tiny board with protruding needles is used. The allergens are placed either on the board or directly on the skin. The board is then placed on the skin, to puncture the skin and for the allergens to enter the body. If a hive appears, the person is considered positive for the allergy. This test only works for IgE antibodies. Allergic reactions caused by other antibodies cannot be detected through skin-prick tests.[63]
Skin-prick testing is easy to do and results are available in minutes. Different allergists may use different devices for testing. Some use a "bifurcated needle", which looks like a fork with two prongs. Others use a "multitest", which may look like a small board with several pins sticking out of it. In these tests, a tiny amount of the suspected allergen is put onto the skin or into a testing device, and the device is placed on the skin to prick, or break through, the top layer of skin. This puts a small amount of the allergen under the skin. A hive will form at any spot where the person is allergic. This test generally yields a positive or negative result. It is good for quickly learning if a person is allergic to a particular food or not because it detects IgE. Skin tests cannot predict if a reaction would occur or what kind of reaction might occur if a person ingests that particular allergen. They can, however, confirm an allergy in light of a patient's history of reactions to a particular food. Non-IgE-mediated allergies cannot be detected by this method.
- Patch testing is used to determine if a specific substance causes allergic inflammation of the skin. It tests for delayed food reactions.[64][65][66]
- Blood testing is another way to test for allergies; however, it poses the same disadvantage and only detects IgE allergens and does not work for every possible allergen. Radioallergosorbent testing (RAST) is used to detect IgE antibodies present to a certain allergen. The score taken from the RAST is compared to predictive values, taken from a specific type of RAST. If the score is higher than the predictive values, a great chance the allergy is present in the person exists. One advantage of this test is that it can test many allergens at one time.[67]
A CAP-RAST has greater specificity than RAST; it can show the amount of IgE present to each allergen.[68] Researchers have been able to determine "predictive values" for certain foods, which can be compared to the RAST results. If a person's RAST score is higher than the predictive value for that food, over a 95% chance exists that patients will have an allergic reaction (limited to rash and anaphylaxis reactions) if they ingest that food. [citation needed] Currently,[when?] predictive values are available for milk, egg, peanut, fish, soy, and wheat.[69][70][71] Blood tests allow for hundreds of allergens to be screened from a single sample, and cover food allergies as well as inhalants. However, non-IgE-mediated allergies cannot be detected by this method. Other widely promoted tests such as the antigen leukocyte cellular antibody test and the food allergy profile are considered unproven methods, the use of which is not advised.[72]
- Food challenges test for allergens other than those caused by IgE allergens. The allergen is given to the person in the form of a pill, so the person can ingest the allergen directly. The person is watched for signs and symptoms. The problem with food challenges is that they must be performed in the hospital under careful watch, due to the possibility of anaphylaxis.[73]
Food challenges, especially double-blind, placebo-controlled food challenges, are the gold standard for diagnosis of food allergies, including most non-IgE-mediated reactions, but is rarely done.[74] Blind food challenges involve packaging the suspected allergen into a capsule, giving it to the patient, and observing the patient for signs or symptoms of an allergic reaction.[medical citation needed]
The recommended method for diagnosing food allergy is to be assessed by an allergist. The allergist will review the patient's history and the symptoms or reactions that have been noted after food ingestion. If the allergist feels the symptoms or reactions are consistent with food allergy, he/she will perform allergy tests. Additional diagnostic tools for evaluation of eosinophilic or non-IgE mediated reactions include endoscopy, colonoscopy, and biopsy.[medical citation needed]
Differential diagnosis
[edit]Important differential diagnoses are:
- Lactose intolerance generally develops later in life, but can present in young patients in severe cases. It is not an immune reaction and is due to an enzyme deficiency (lactase). It is more common in many non-Western people.
- Celiac disease. While it is caused by a permanent intolerance to gluten (present in wheat, rye, barley and oats), is not an allergy nor simply an intolerance, but a chronic, multiple-organ autoimmune disorder primarily affecting the small intestine.[75][76][77]
- Irritable bowel syndrome
- C1 Esterase inhibitor deficiency (hereditary angioedema), a rare disease, generally causes attacks of angioedema, but can present solely with abdominal pain and occasional diarrhea, and thus may be confused with allergy-triggered angioedema.
Prevention
[edit]Breastfeeding for more than four months may prevent atopic dermatitis, cow's milk allergy, and wheezing in early childhood.[78] Early exposure to potential allergens may be protective.[2] Specifically, early exposure to eggs and peanuts reduces the risk of allergies to these.[3] Guidelines suggest introducing peanuts as early as 4–6 months and include precautionary measures for high-risk infants.[79] The former guidelines, advising delaying the introduction of peanuts, are now[when?] thought to have contributed to the increase in peanut allergy seen recently.[80][better source needed]
To avoid an allergic reaction, a strict diet can be followed. It is difficult to determine the amount of allergenic food required to elicit a reaction, so complete avoidance should be attempted. In some cases, hypersensitive reactions can be triggered by exposures to allergens through skin contact, inhalation, kissing, participation in sports, blood transfusions, cosmetics, and alcohol.[81]
Early introduction of peanut and egg alongside other solids, or by one year of age, may help prevent development of food allergy. Introduction of these allergenic foods within the first year of life appears to be safe. A window of opportunity for the introduction of different food allergens may exist, such as egg introduction ahead of peanut.[82]
Inhalation exposure
[edit]Allergic reactions to airborne particles or vapors of known food allergens have been reported as an occupational consequence of people working in the food industry, but can also take place in home situations, restaurants, or confined spaces such as airplanes. According to two reviews, respiratory symptoms are common, but in some cases there has been progression to anaphylaxis.[83][84] The most frequent reported cases of reactions by inhalation of allergenic foods were due to peanut, seafood, legumes, tree nut, and cow's milk.[83] Steam rising from cooking of lentils, green beans, chickpeas and fish has been well documented as triggering reactions, including anaphylactic reactions.[83][85] One review mentioned case study examples of allergic responses to inhalation of other foods, including examples in which oral consumption of the food is tolerated.[83]
Treatment
[edit]The mainstay of treatment for food allergy is total avoidance of the foods identified as allergens. An allergen can enter the body by consuming a portion of food containing the allergen, and can also be ingested by touching any surfaces that may have come into contact with the allergen, then touching the eyes or nose. For people who are extremely sensitive, avoidance includes avoiding touching or inhaling problematic food. Total avoidance is complicated because the declaration of the presence of trace amounts of allergens in foods is not mandatory (see regulation of labelling).
If the food is accidentally ingested and a systemic reaction (anaphylaxis) occurs, then epinephrine should be used. A second dose of epinephrine may be required for severe reactions. The person should then be transported to the emergency room, where additional treatment can be given. Other treatments include antihistamines and steroids.[86]
Epinephrine
[edit]
Epinephrine (adrenaline) is the first-line treatment for severe allergic reactions (anaphylaxis). If administered in a timely manner, epinephrine can reverse its effects. Epinephrine relieves airway swelling and obstruction, and improves blood circulation; blood vessels are tightened and heart rate is increased, improving circulation to body organs. Epinephrine is available by prescription in an autoinjector.[87]
Antihistamines
[edit]Antihistamines can alleviate some of the milder symptoms of an allergic reaction, but do not treat all symptoms of anaphylaxis.[88] Antihistamines block the action of histamine, which causes blood vessels to dilate and become leaky to plasma proteins. Histamine also causes itchiness by acting on sensory nerve terminals. The most common antihistamine given for food allergies is diphenhydramine.
Steroids
[edit]Glucocorticoid steroids are used to calm down the immune system cells that are attacked by the chemicals released during an allergic reaction. This treatment in the form of a nasal spray should not be used to treat anaphylaxis, for it only relieves symptoms in the area in which the steroid is in contact. Another reason steroids should not be used is the delay in reducing inflammation. Steroids can also be taken orally or through injection, by which every part of the body can be reached and treated, but a long time is usually needed for these to take effect.[89]
Immunotherapy
[edit]Immunotherapies seek to condition the immune system to elicit or suppress a specific immune response. In the treatment of allergies, common immunotherapies seek to desensitize the immune system by gradually exposing the body to allergens in increasing amounts. These forms of immunotherapy have had varying and limited success and have generally been used to treat peanut and environmental allergies.[90]
Omalizumab
[edit]Omalizumab, an injectable asthma treatment drug sold under the brand name Xolair, was approved in the United States in February 2024 to reduce severe reactions to accidental exposure to food allergens.[91] It is a genetically engineered monoclonal antibody which specifically binds to immunoglobulin E (IgE) to reduce the severity of an immune response. Successful results were reported for wheat, eggs, milk and baked products containing wheat and milk.[92]
Epidemiology
[edit]Food allergies affect up to 10% of the worldwide population, and they are currently more prevalent in children (~8%) than adults (~5) in western nations.[34] In several industrialized countries, food allergies affect up to 10% of children.[93] Children are most commonly allergic to cow's milk, chicken eggs, peanuts, and tree nuts.[21] While studies on adults with food allergy are not as abundant, surveys suggest that the most common food allergens for adults include fish, shellfish, peanuts, and tree nuts.[93]
Food allergies have become increasingly prevalent in industrialized/westernized nations over the last 2–3 decades.[94] An estimated 15 million people currently have food allergies in the United States.[95] In 1997, 0.4% children in the United States were reported to have peanut allergy, yet this number markedly rose to 1.4% in 2008.[96] In Australia, hospital admission rates for food-induced anaphylaxis increased by an average of 13.2% from 1994-2005.[93] One possible explanation for the rise in food allergy is the "old friends" hypothesis, which suggests that non-disease-causing organisms, such as helminths, could protect against allergy. Therefore, reduced exposure to these organisms, particularly in developed countries, could have contributed towards the increase.[citation needed]
Children of East Asian or African descent who live in westernized countries were reported to be at significantly higher risk of food allergy compared to Caucasian children.[15] Several studies predict that Asia and Africa may experience a growth in food allergy prevalence as the lifestyles there become more westernized.[93]
The prevalence of certain food allergies is suggested to depend partly on the geographical area and country. For instance, allergy to buckwheat flour, used for soba noodles, is more common in Japan than peanuts, tree nuts or foods made from soy beans.[97] Also, shellfish allergy is the most common cause of anaphylaxis in adults and adolescents particularly in East Asian countries like Hong Kong, Taiwan, Singapore, and Thailand.[93] Individuals in East Asia have further developed an allergy to rice, which forms a large part of their diet.[98] Another example is that, out of nine European countries, egg allergy was found[by whom?] to be most prevalent in the UK and least prevalent in Greece.[citation needed]
Special population: children
[edit]About 75% of children who have allergies to milk protein are able to tolerate baked-in milk products, i.e., muffins, cookies, cake, and hydrolyzed formulas.[99] About 50% of children with allergies to milk, egg, soy, peanuts, tree nuts, and wheat will outgrow their allergy by the age of 6. Those who are still allergic by the age of 12 or so have less than an 8% chance of outgrowing the allergy.[100]
United States
[edit]In the United States, food allergy affects as many as 5% of infants less than three years of age[101] and 3% to 4% of adults.[102][103] The prevalence of food allergies is rising.[104][105][106] Food allergies cause roughly 30,000 emergency room visits and 150 deaths per year.[107]
Regulation
[edit]Whether rates of food allergy are increasing or not, food allergy awareness has definitely increased, with impacts on the quality of life for children, their parents and their caregivers.[108][109][110][111] In the United States, the Food Allergen Labeling and Consumer Protection Act of 2004 causes people to be reminded of allergy problems every time they handle a food package, and restaurants have added allergen warnings to menus. The Culinary Institute of America, a premier school for chef training, has courses in allergen-free cooking and a separate teaching kitchen.[112] School systems have protocols about what foods can be brought into the school. Despite all these precautions, people with serious allergies are aware that accidental exposure can easily occur at other peoples' houses, at school or in restaurants.[113]
Regulation of labelling
[edit]
In response to the risk that certain foods pose to those with food allergies, some countries have responded by instituting labeling laws that require food products to clearly inform consumers if their products contain priority allergens or byproducts of major allergens among the ingredients intentionally added to foods.
The priority allergens vary by country.
| Food | US | Canada | UK | Australia & New Zealand | EU |
|---|---|---|---|---|---|
| peanuts | Yes[114] | Yes[115] | Yes[116] | Yes[117] | Yes[118] |
| tree nuts | Yes[114] | Yes[115] | Yes[116] | Almonds, Brazil nuts, cashews, hazelnuts, macadamias, pecans, pistachios, pine nuts, and walnuts.[117] | Yes[118] |
| milk | Yes[114] | Yes[115] | Yes[116] | Yes[117] | Yes[118] |
| eggs | Yes[114] | Yes[115] | Yes[116] | Yes[117] | Yes[118] |
| fish | Yes[114] | Yes[115] | Yes[116] | Yes[117] | Yes[118] |
| shellfish | Crustaceans only[114] | Crustaceans and molluscs[115] | Crustaceans and molluscs[116] | Crustaceans and molluscs[117] | Crustaceans and molluscs[118] |
| soy | Yes[114] | Yes[115] | Yes[116] | Yes[117] | Yes[118] |
| wheat | Yes[114] | Includes triticale[115] | Included under gluten[116] | Yes[117] | Included under gluten[118] |
| sesame seeds | Yes as of 2023[119] | Yes[115] | Yes[116] | Yes[117] | Yes[118] |
| mustard | No | Yes[115] | Yes[116] | No | Yes[118] |
| sulphites (not a true allergy) | No | Yes[115] | Yes[116] | Yes, if >10 mg/kg[117] | Yes, if >10 mg/kg[118] |
| gluten (not a true allergy) | No | Yes[115] | Yes[116] | Yes[117] | Yes[118] |
| celery | No | No | Yes[116] | No | Yes[118] |
| lupin | No | No | Yes[116] | Yes[117] | Yes[118] |
There are no labeling laws mandating declaration of the presence of trace amounts in the final product as a consequence of cross-contamination, except in Brazil.[120][121][122][123][124][125][126][127]
Ingredients intentionally added
[edit]In the United States, the Food Allergen Labeling and Consumer Protection Act of 2004 requires companies to disclose on the label whether a packaged food product contains any of these eight major food allergens, added intentionally: cow's milk, peanuts, eggs, shellfish, fish, tree nuts, soy and wheat.[121] The eight-ingredient list originated in 1999 from the World Health Organisation Codex Alimentarius Commission.[126] To meet labeling requirements, if an ingredient is derived from one of the required-label allergens, then it must either have its "food sourced name" in parentheses, for example, "Casein (milk)," or as an alternative, there must be a statement separate but adjacent to the ingredients list: "Contains milk" (and any other of the allergens with mandatory labeling).[121][123] The European Union requires listing for those eight major allergens plus molluscs, celery, mustard, lupin, sesame and sulfites.[122]
In 2018, the US FDA issued a request for information for the consideration of labeling for sesame to help protect people who have sesame allergies.[128] A decision was reached in November 2020 that food manufacturers voluntarily declare that when powdered sesame seeds are used as a previously unspecified spice or flavor, the label be changed to "spice (sesame)" or "flavor (sesame)."[129]
Congress and the President passed a law in April 2021, the "FASTER Act", stipulating that labeling be mandatory, to be effect January 1, 2023, making it the ninth required food ingredient label.[130]
The Food Allergen Labeling and Consumer Protection Act of 2004 applies to packaged foods regulated by the FDA, which does not include poultry, most meats, certain egg products, and most alcoholic beverages.[127] However, some meat, poultry, and egg processed products may contain allergenic ingredients. These products are regulated by the Food Safety and Inspection Service, which requires that any ingredient be declared in the labeling only by its common or usual name. Neither the identification of the source of a specific ingredient in a parenthetical statement nor the use of statements to alert for the presence of specific ingredients, like "Contains: milk", are mandatory.[124][125] The act also does not apply to food prepared in restaurants.[131][132] The EU Food Information for Consumers Regulation 1169/2011 – requires food businesses to provide allergy information on food sold unpackaged, for example, in catering outlets, deli counters, bakeries and sandwich bars.[133]
In the United States, there is no federal mandate to address the presence of allergens in drug products, medicines, or cosmetics.[134]
Trace amounts as a result of cross-contamination
[edit]The value of allergen labeling other than for intentional ingredients is controversial. This concerns labeling for ingredients present unintentionally as a consequence of cross-contact or cross-contamination at any point along the food chain (during raw material transportation, storage or handling, due to shared equipment for processing and packaging, etc.).[126][127] Experts in this field propose that if allergen labeling is to be useful to consumers, and healthcare professionals who advise and treat those consumers, ideally there should be agreement on which foods require labeling, threshold quantities below which labeling may be of no purpose, and validation of allergen detection methods to test and potentially recall foods that were deliberately or inadvertently contaminated.[135][136]
Labeling regulations have been modified to provide for mandatory labeling of ingredients plus voluntary labeling, termed precautionary allergen labeling, also known as "may contain" statements, for possible, inadvertent, trace amount, cross-contamination during production.[126][137] Precautionary allergen labeling can be confusing to consumers, especially as there can be many variations on the wording of the warning.[137][138] Precautionary allergen labeling is optional in the United States.[139] As of 2014[update], precautionary allergen labeling is regulated only in Switzerland, Japan, Argentina, and South Africa. Argentina decided to prohibit precautionary allergen labeling since 2010 and instead puts the onus on the manufacturer to control the manufacturing process and label only those allergenic ingredients known to be in the products. South Africa does not permit the use of precautionary allergen labeling, except when manufacturers demonstrate the potential presence of allergen due to cross-contamination through a documented risk assessment and despite adherence to Good Manufacturing Practice.[126] In Australia and New Zealand there is a recommendation that precautionary allergen labeling be replaced by guidance from VITAL 2.0 (Vital Incidental Trace Allergen Labeling). A review identified "the eliciting dose for an allergic reaction in 1% of the population" as the threshold reference dose for certain foods (such as cow's milk, egg, peanut and other proteins) to provide food manufacturers with guidance for developing precautionary labeling and give consumers a better idea of what might be accidentally in a food product beyond "may contain."[140][141] VITAL 2.0 was developed by the Allergen Bureau, a food industry sponsored, non-government organization.[142] The European Union has initiated a process to create labeling regulations for unintentional contamination but is not expected to publish such before 2024.[143]
In Brazil, since April 2016, the declaration of the possibility of cross-contamination is mandatory when the product does not intentionally add any allergenic food or its derivatives, but the Good Manufacturing Practices and allergen control measures adopted are not sufficient to prevent the presence of accidental trace amounts. These allergens include wheat, rye, barley, oats and their hybrids, crustaceans, eggs, fish, peanuts, soybean, milk of all species of mammalians, almonds, hazelnuts, cashew nuts, Brazil nuts, macadamia nuts, walnuts, pecan nuts, pistachios, pine nuts, and chestnuts.[120]
Genetically modified food
[edit]There is a scientific consensus that available food derived from genetically modified crops poses no greater risk to human health than conventional food,[144][145][146] and a 2016 U.S. National Academy of Sciences report concluded that there is no relationship between consumption of genetically modified foods and the increase in prevalence of food allergies.[147] However, there are concerns that genetically modified foods, also described as foods sourced from genetically modified organisms, could be responsible for allergic reactions, and that the widespread acceptance of these types of foods may be responsible for what is a real or perceived increase in the percentage of people with allergies.[148][147][149]
One concern is that genetic engineering could make an allergy-provoking food more allergic, meaning that smaller portions would suffice to set off a reaction.[149] Of the food currently[when?] in widespread use of genetically modified organisms, only soybeans are identified as a common allergen. However, for the soybean proteins known to trigger allergic reactions, there is more variation from strain to strain than between those and the genetically modified varieties.[147] Another concern is that genes transferred from one species to another could introduce an allergen in a food not thought of as particularly allergenic. Research on an attempt to enhance the quality of soybean protein by adding genes from Brazil nuts was terminated when human volunteers known to have tree nut allergy reacted to the modified soybeans.[148]
Prior to a new genetically modified food receiving government approval, certain criteria need to be met. These include: Is the donor species known to be allergenic? Does the amino acid sequence of the transferred proteins resemble the sequence of known allergenic proteins? Are the transferred proteins resistant to digestion – a trait shared by many allergenic proteins?[147] Genes approved for animal use can be restricted from human consumption due to potential for allergic reactions. In 1998 StarLink brand corn restricted to animals was detected in the human food supply, leading to first a voluntary and then an FDA-mandated recall.[150] There are requirements in some countries and recommendations in others that all foods containing genetically modified ingredients be so labeled, and that there be a post-launch monitoring system to report adverse effects (similar to the requirements in some countries for drug and dietary supplement reporting).[148]
Restaurants
[edit]In the US, the FDA Food Code states that the person in charge in restaurants should have knowledge about major food allergens, cross-contacts, and symptoms of food allergy reactions. Restaurant staff, including wait staff and kitchen staff, may not be adequately informed about allergenic ingredients, or the risk of cross-contact when kitchen utensils used to prepare food may have been in previous contact with an allergenic food. The problem may be compounded when customers have a hard time describing their food allergies or when wait staff have a hard time understanding those with food allergies when taking an order.[151]
Diagnosing issues
[edit]There exists both over-reporting and under-reporting of the prevalence of food allergies. Self-diagnosed perceptions of food allergy are greater than the rates of true food allergy because people confuse non-allergic intolerance with allergy, and also attribute non-allergy symptoms to an allergic response. Conversely, healthcare professionals treating allergic reactions on an out-patient or even hospitalized basis may not report all cases. Recent increases in reported cases may reflect a real change in incidence or an increased awareness on the part of healthcare professionals.[152]
Social impact
[edit]Food fear has a significant impact on quality of life.[110][111] For children with allergies, their quality of life is also affected by the actions of their peers. An increased occurrence of bullying has been observed, which can include threats or deliberate acts of forcing allergic children to contact foods that they must avoid or intentional contamination of allergen-free food.[153] The social impacts of food allergies can carry over into adulthood.[154]
Portrayal in media
[edit]Media portrayals of food allergy in television and film are not accurate, often used for comedic effect or underplaying the potential severity of an allergic reaction.[155] These tropes misinform the public and also contribute to how entertainment media will continue to wrongly portray food allergies in the future. Types of tropes: 1) characters have food allergies, providing a weakness that can be used to sabotage them. In the movie Parasite a housekeeper is displaced by taking advantage of her peach allergy.[156] In the animated film Peter Rabbit, the farm owner is attacked by being pelted with blackberries, causing an anaphylactic reaction requiring emergency treatment with epinephrine. After many public protests, Sony Pictures and the Peter Rabbit director apologized for making light of food allergies.[157] 2) Food allergy is used for comedic effect, such as in the movies Hitch and in television, Kelso's egg allergy in That '70s Show. 3) Food allergies may be incorporated into characters who are also portrayed as annoying, weak and oversensitive, which can be taken as implying that their allergies are either not real or not potentially severe. In season 1, episode 16 of The Big Bang Theory Howard Wolowitz deliberately consumes a peanut-containing food bar (and has a serious reaction) just to delay Leonard from returning to his apartment where a surprise birthday party is being arranged. 4) Any of these portrayals may underplay the potential severity of food allergy, some showing that Benadryl treatment is sufficient.[156] Viewing of humorous portrayals of food allergies has been shown to have a negative effect on related health policy support due to low perceived seriousness.[155]
Research
[edit]Several theories have been suggested to explain why certain individuals develop allergic sensitization instead of oral tolerance to food allergens. One such theory is the dual allergen hypothesis, which states that ingesting food allergens early on promotes oral tolerance while skin exposure leads to sensitization.[95] Instead of oral ingestion, skin barrier disruption in conditions like eczema, for instance, was suggested to cause allergic sensitization in animal and human infants.[48] Inhalation was recently proposed to be an additional sensitization route in the dual allergen hypothesis.[42] Another theory is the barrier regulation hypothesis, describing the role of commensal bacteria in preventing the development of food allergy by maintaining integrity of the intestinal epithelial barrier.[95] Environmental and lifestyle factors, such as early life nutrition and antibiotic treatment, may contribute to food allergy prevalence by affecting gut microbial composition, and thus, intestinal immune homeostasis in infants and young children.[158]
A number of desensitization techniques are being studied.[159] Areas of research include specific oral tolerance induction (also known as oral immunotherapy), and sublingual immunotherapy. The benefits of allergen immunotherapy for food allergies is unclear, thus is not recommended as of 2015[update].[7]
There is research on the effects of increasing intake of polyunsaturated fatty acids during pregnancy, lactation, via infant formula and in early childhood on the subsequent risk of developing food allergies during infancy and childhood. From two reviews, maternal intake of omega-3, long-chain fatty acids during pregnancy appeared to reduce the risks of medically diagnosed IgE-mediated allergy, eczema and food allergy per parental reporting in the first 12 months of life,[160][161] but the effects were not all sustained past 12 months.[161] The reviews characterized the literature's evidence as inconsistent and limited.[160][161] Results when breastfeeding mothers were consuming a diet high in polyunsaturated fatty acids were inconclusive.[162] For infants, supplementing their diet with oils high in polyunsaturated fatty acids did not affect the risks of food allergies, eczema or asthma either as infants or into childhood.[163]
There is research on probiotics, prebiotics and the combination of the two (synbiotics) as a means of treating or preventing infant and child allergies. From reviews, there appears to be a treatment benefit for eczema,[164][165][166] but not asthma, wheezing or rhinoconjunctivitis.[167] The evidence was not consistent for preventing food allergies and this approach cannot yet be recommended.[165][166][168][169]
The Food Standards Agency, in the United Kingdom, are in charge of funding research into food allergies and intolerance.[152] Since their founding in 1994 they have funded over 45 studies.[152] In 2005 Europe created EuroPrevall, a multi-country project dedicated to research involving allergies.[152]
See also
[edit]- List of allergens (food and non-food)
References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t u National Institute of Allergy and Infectious Diseases (July 2012). "Food Allergy An Overview" (PDF). Archived from the original (PDF) on 5 March 2016.
- ^ a b c d e f g h i j k l m n o p q r Sicherer SH, Sampson HA (February 2014). "Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment". The Journal of Allergy and Clinical Immunology. 133 (2): 291–307, quiz 308. doi:10.1016/j.jaci.2013.11.020. PMID 24388012.
- ^ a b c Ierodiakonou D, Garcia-Larsen V, Logan A, Groome A, Cunha S, Chivinge J, et al. (September 2016). "Timing of Allergenic Food Introduction to the Infant Diet and Risk of Allergic or Autoimmune Disease: A Systematic Review and Meta-analysis". JAMA. 316 (11): 1181–1192. doi:10.1001/jama.2016.12623. hdl:10044/1/40479. PMID 27654604.
- ^ Boyce JA, Assa'ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. (December 2010). "Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the NIAID-Sponsored Expert Panel Report". The Journal of Allergy and Clinical Immunology. 126 (6): 1105–1118. doi:10.1016/j.jaci.2010.10.008. PMC 4241958. PMID 21134568.
- ^ Sicherer SH, Sampson HA (January 2018). "Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management". The Journal of Allergy and Clinical Immunology. 141 (1): 41–58. doi:10.1016/j.jaci.2017.11.003. PMID 29157945.
- ^ Nowak-Węgrzyn A, Katz Y, Mehr SS, Koletzko S (May 2015). "Non-IgE-mediated gastrointestinal food allergy". The Journal of Allergy and Clinical Immunology. 135 (5): 1114–1124. doi:10.1016/j.jaci.2015.03.025. PMID 25956013.
- ^ a b "Allergen Immunotherapy". 22 April 2015. Archived from the original on 17 June 2015. Retrieved 15 June 2015.
- ^ "Making sense of allergies" (PDF). Sense About Science. p. 1. Archived from the original (PDF) on 18 June 2015. Retrieved 7 June 2015.
- ^ Coon ER, Quinonez RA, Moyer VA, Schroeder AR (November 2014). "Overdiagnosis: how our compulsion for diagnosis may be harming children". Pediatrics. 134 (5): 1013–1023. doi:10.1542/peds.2014-1778. PMID 25287462.
- ^ Ferreira CT, Seidman E (2007). "Food allergy: a practical update from the gastroenterological viewpoint". Jornal de Pediatria. 83 (1): 7–20. doi:10.2223/JPED.1587. PMID 17279290.
- ^ a b c d e f g h i j k l m n MedlinePlus Encyclopedia: Food allergy
- ^ Simons FE, Ardusso LR, Bilò MB, El-Gamal YM, Ledford DK, Ring J, et al. (February 2011). "World allergy organization guidelines for the assessment and management of anaphylaxis". The World Allergy Organization Journal. 4 (2): 13–37. doi:10.1097/WOX.0b013e318211496c. PMC 3500036. PMID 23268454.
- ^ van Ree 1
- ^ Sicherer 2006, p. 12
- ^ a b Sicherer SH, Sampson HA (January 2018). "Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management". The Journal of Allergy and Clinical Immunology. 141 (1): 41–58. doi:10.1016/j.jaci.2017.11.003. PMID 29157945.
- ^ "Food Allergy Research & Education". 9 December 2013. Archived from the original on 9 December 2013. Retrieved 2 December 2022.
- ^ "Food Allergy Facts & Figures". Asthma and Allergy Foundation of America. 28 March 2007. Archived from the original on 7 December 2006. Retrieved 15 March 2007.
- ^ "Food allergy and intolerance". Allergy & Intolerance. Food Additives and Ingredients Association. Archived from the original on 13 February 2011. Retrieved 8 June 2010.
- ^ Center for Food Safety and Applied Nutrition (22 June 2022). "Food Allergies". FDA. Retrieved 31 July 2022.
- ^ "In April of 2021, President Joe Biden signed the FASTER Act into law". www.bing.com. Retrieved 1 January 2023.
- ^ a b Sampson HA, Burks AW (July 1996). "Mechanisms of food allergy". Annual Review of Nutrition. 16 (1): 161–177. doi:10.1146/annurev.nu.16.070196.001113. PMID 8839924.
- ^ Lieberman JA, Gupta RS, Knibb RC, Haselkorn T, Tilles S, Mack DP, Pouessel G (May 2021). "The global burden of illness of peanut allergy: A comprehensive literature review". Allergy. 76 (5): 1367–1384. doi:10.1111/all.14666. PMC 8247890. PMID 33216994.
- ^ a b Sicherer 2006, p. 63
- ^ Fleischer DM, Conover-Walker MK, Matsui EC, Wood RA (November 2005). "The natural history of tree nut allergy". The Journal of Allergy and Clinical Immunology. 116 (5): 1087–1093. doi:10.1016/j.jaci.2005.09.002. PMID 16275381.
- ^ Savage JH, Matsui EC, Skripak JM, Wood RA (December 2007). "The natural history of egg allergy". The Journal of Allergy and Clinical Immunology. 120 (6): 1413–1417. doi:10.1016/j.jaci.2007.09.040. PMID 18073126.
- ^ Dona DW, Suphioglu C (July 2020). "Egg Allergy: Diagnosis and Immunotherapy". International Journal of Molecular Sciences. 21 (14): 5010. doi:10.3390/ijms21145010. PMC 7404024. PMID 32708567.
- ^ Flom JD, Sicherer SH (May 2019). "Epidemiology of Cow's Milk Allergy". Nutrients. 11 (5): 1051. doi:10.3390/nu11051051. PMC 6566637. PMID 31083388.
- ^ Ogata M, Kido J, Nakamura K (October 2021). "Oral Immunotherapy for Children with Cow's Milk Allergy". Pathogens. 10 (10): 1328. doi:10.3390/pathogens10101328. PMC 8539286. PMID 34684278.
- ^ Sicherer 2006, p. 64
- ^ Wang HT, Warren CM, Gupta RS, Davis CM (April 2020). "Prevalence and Characteristics of Shellfish Allergy in the Pediatric Population of the United States". The Journal of Allergy and Clinical Immunology. In Practice. 8 (4): 1359–1370.e2. doi:10.1016/j.jaip.2019.12.027. PMC 7951995. PMID 31917365.
- ^ "Seafood (Fish, Crustaceans and Shellfish) - Priority food allergens". Health Canada, Health Products and Food Branch, Food Directorate, Bureau of Chemical Safety, Food Research Division. 2012. Archived from the original on 20 November 2016. Retrieved 19 November 2016.
- ^ Kalic T, Radauer C, Lopata AL, Breiteneder H, Hafner C (2021). "Fish Allergy Around the World-Precise Diagnosis to Facilitate Patient Management". Frontiers in Allergy. 2: 732178. doi:10.3389/falgy.2021.732178. PMC 8974716. PMID 35387047.
- ^ a b Iweala OI, Choudhary SK, Commins SP (April 2018). "Food Allergy". Current Gastroenterology Reports. 20 (5): 17. doi:10.1007/s11894-018-0624-y. PMC 5940350. PMID 29623490.
- ^ a b c d e f Sathe SK, Liu C, Zaffran VD (28 February 2016). "Food Allergy". Annual Review of Food Science and Technology. 7 (1): 191–220. doi:10.1146/annurev-food-041715-033308. PMID 26934173.
- ^ Skypala IJ (2019). "Food-Induced Anaphylaxis: Role of Hidden Allergens and Cofactors". Frontiers in Immunology. 10: 673. doi:10.3389/fimmu.2019.00673. PMC 6457317. PMID 31001275.
- ^ Andreozzi L, Giannetti A, Cipriani F, Caffarelli C, Mastrorilli C, Ricci G (January 2019). "Hypersensitivity reactions to food and drug additives: problem or myth?". Acta Bio-Medica. 90 (3–S): 80–90. doi:10.23750/abm.v90i3-S.8168. PMC 6502174. PMID 30830065.
- ^ Gottfried Schmalz; Dorthe Arenholt Bindslev (2008). Biocompatibility of Dental Materials. Springer. ISBN 9783540777823. Archived from the original on 18 May 2016. Retrieved 5 March 2014.
- ^ Yoo Y, Perzanowski MS (October 2014). "Allergic sensitization and the environment: latest update". Current Allergy and Asthma Reports. 14 (10): 465. doi:10.1007/s11882-014-0465-1. PMC 6421846. PMID 25149167.
- ^ Valenta R, Hochwallner H, Linhart B, Pahr S (May 2015). "Food allergies: the basics". Gastroenterology. 148 (6): 1120–31.e4. doi:10.1053/j.gastro.2015.02.006. PMC 4414527. PMID 25680669.
- ^ a b Johnson RM, Barnes CS (2013). "Airborne concentrations of peanut protein". Allergy and Asthma Proceedings. 34 (1): 59–64. doi:10.2500/aap.2013.34.3622. PMID 23406937.
- ^ a b Foong RX, Brough H (October 2017). "The role of environmental exposure to peanut in the development of clinical allergy to peanut". Clinical and Experimental Allergy. 47 (10): 1232–1238. doi:10.1111/cea.12992. PMID 28779526. S2CID 10119958.
- ^ a b c Kulis MD, Smeekens JM, Immormino RM, Moran TP (September 2021). "The airway as a route of sensitization to peanut: An update to the dual allergen exposure hypothesis". The Journal of Allergy and Clinical Immunology. 148 (3): 689–693. doi:10.1016/j.jaci.2021.05.035. PMC 8429226. PMID 34111450.
- ^ a b c Lopata AL, Jeebhay MF (June 2013). "Airborne seafood allergens as a cause of occupational allergy and asthma". Current Allergy and Asthma Reports. 13 (3): 288–297. doi:10.1007/s11882-013-0347-y. PMID 23575656. S2CID 1276304.
- ^ Ramirez DA, Bahna SL (February 2009). "Food hypersensitivity by inhalation". Clinical and Molecular Allergy. 7 (1): 4. doi:10.1186/1476-7961-7-4. PMC 2651849. PMID 19232116.
- ^ Jeebhay MF, Robins TG, Lehrer SB, Lopata AL (September 2001). "Occupational seafood allergy: a review". Occupational and Environmental Medicine. 58 (9): 553–562. doi:10.1136/oem.58.9.553. PMC 1740192. PMID 11511741.
- ^ Brant A (April 2007). "Baker's asthma". Current Opinion in Allergy and Clinical Immunology. 7 (2): 152–155. doi:10.1097/ACI.0b013e328042ba77. PMID 17351468. S2CID 24085274.
- ^ Saygin D, Tabib T, Bittar HE, Valenzi E, Sembrat J, Chan SY, et al. (1976). "Transcriptional profiling of lung cell populations in idiopathic pulmonary arterial hypertension". Pulmonary Circulation. 10 (1): 392–406. doi:10.1177/2045894020908782. PMC 7052475. PMID 32166015.
- ^ a b Calvani M, Anania C, Caffarelli C, Martelli A, Miraglia Del Giudice M, Cravidi C, et al. (September 2020). "Food allergy: an updated review on pathogenesis, diagnosis, prevention and management". Acta Bio-Medica. 91 (11–S): e2020012. doi:10.23750/abm.v91i11-S.10316. PMC 8023067. PMID 33004782.
- ^ Thompson RL, Miles LM, Lunn J, Devereux G, Dearman RJ, Strid J, Buttriss JL (May 2010). "Peanut sensitisation and allergy: influence of early life exposure to peanuts". The British Journal of Nutrition. 103 (9): 1278–1286. doi:10.1017/S000711450999376X. PMID 20100372. S2CID 3619861.
- ^ a b Brough HA, Nadeau KC, Sindher SB, Alkotob SS, Chan S, Bahnson HT, et al. (September 2020). "Epicutaneous sensitization in the development of food allergy: What is the evidence and how can this be prevented?". Allergy. 75 (9): 2185–2205. doi:10.1111/all.14304. PMC 7494573. PMID 32249942.
- ^ "Other atopic dermatitis and related conditions". ICD9. Archived from the original on 30 September 2007.
- ^ "Policy Statement: Hypoallergenic Infant Formulas". American Academy of Pediatrics. 2 August 2000. Archived from the original on 16 January 2008. Retrieved 26 January 2008.
- ^ Sicherer, SH; Noone, SA; Koerner, CB; Christie, L; Burks, AW; Sampson, HA (May 2001). "Hypoallergenicity and efficacy of an amino acid–based formula in children with cow's milk and multiple food hypersensitivities". The Journal of Pediatrics. 138 (5): 688–93. doi:10.1067/mpd.2001.113007. ISSN 0022-3476. PMID 11343044.
- ^ Lopata AL, Kleine-Tebbe J, Kamath SD (2016). "Allergens and molecular diagnostics of shellfish allergy: Part 22 of the Series Molecular Allergology". Allergo Journal International. 25 (7): 210–218. doi:10.1007/s40629-016-0124-2. PMC 5306157. PMID 28239537.
- ^ "Other Common Allergens". Food Allergy Research & Education. Archived from the original on 16 June 2014. Retrieved 12 June 2014.
- ^ "Food allergy". NHS Choices. 16 May 2016. Retrieved 31 January 2017.
A food allergy is when the body's immune system reacts unusually to specific foods
- ^ Food Reactions. Allergies Archived 2010-04-16 at the Wayback Machine. Foodreactions.org. Kent, England. 2005. Accessed 27 Apr 2010.
- ^ Nester 2009, p. 414
- ^ Mayo Clinic. Causes of Food Allergies. Archived 2010-02-27 at the Wayback Machine April 2010.
- ^ a b Janeway C, Travers P, Walport M, Shlomchik M (2001). Immunobiology; Fifth Edition. New York and London: Garland Science. pp. e–book. ISBN 978-0-8153-4101-7. Archived from the original on 28 June 2009.
- ^ Grimbaldeston MA, Metz M, Yu M, Tsai M, Galli SJ (December 2006). "Effector and potential immunoregulatory roles of mast cells in IgE-associated acquired immune responses". Current Opinion in Immunology. 18 (6): 751–760. doi:10.1016/j.coi.2006.09.011. PMID 17011762.
- ^ Holt PG, Sly PD (October 2007). "Th2 cytokines in the asthma late-phase response". Lancet. 370 (9596): 1396–1398. doi:10.1016/S0140-6736(07)61587-6. PMID 17950849. S2CID 40819814.
- ^ Sicherer 2006, p. 185
- ^ "Allergies and EGIDs | American Partnership For Eosinophilic Disorders". Apfed.org. Archived from the original on 4 May 2015. Retrieved 31 March 2014.
- ^ "Patch test in the diagnosis of food allergy". 22 March 2014. Archived from the original on 10 March 2014. Retrieved 31 March 2014.
- ^ Rokaite R, Labanauskas L, Vaideliene L (24 January 2014). "Role of the skin patch test in diagnosing food allergy in children with atopic dermatitis". Medicina. 40 (11): 1081–1087. PMID 15547309.
- ^ Sicherer 2006, pp. 187–8
- ^ "What is a RAST test ? What is a CAP-RAST test?". kidswithfoodallergies.org. Archived from the original on 11 May 2013.
- ^ Sampson HA, Ho DG (October 1997). "Relationship between food-specific IgE concentrations and the risk of positive food challenges in children and adolescents". The Journal of Allergy and Clinical Immunology. 100 (4): 444–451. doi:10.1016/S0091-6749(97)70133-7. PMID 9338535.
- ^ Sampson HA (May 2001). "Utility of food-specific IgE concentrations in predicting symptomatic food allergy". The Journal of Allergy and Clinical Immunology. 107 (5): 891–896. doi:10.1067/mai.2001.114708. PMID 11344358.
- ^ García-Ara C, Boyano-Martínez T, Díaz-Pena JM, Martín-Muñoz F, Reche-Frutos M, Martín-Esteban M (January 2001). "Specific IgE levels in the diagnosis of immediate hypersensitivity to cows' milk protein in the infant". The Journal of Allergy and Clinical Immunology. 107 (1): 185–190. doi:10.1067/mai.2001.111592. PMID 11150010.
- ^ Wüthrich B (2005). "Unproven techniques in allergy diagnosis". Journal of Investigational Allergology & Clinical Immunology. 15 (2): 86–90. PMID 16047707.
- ^ Sicherer 2006, p. 189
- ^ Turnbull JL, Adams HN, Gorard DA (January 2015). "Review article: the diagnosis and management of food allergy and food intolerances". Alimentary Pharmacology & Therapeutics (Review). 41 (1): 3–25. doi:10.1111/apt.12984. PMID 25316115. S2CID 31761992.

- ^ "Celiac Disease". NIDDKD. June 2015. Archived from the original on 13 March 2016. Retrieved 17 March 2016.
- ^ "Celiac disease". World Gastroenterology Organisation Global Guidelines. July 2016. Archived from the original on 17 March 2017. Retrieved 23 April 2017.
- ^ Tommasini A, Not T, Ventura A (August 2011). "Ages of celiac disease: from changing environment to improved diagnostics". World Journal of Gastroenterology (Review). 17 (32): 3665–3671. doi:10.3748/wjg.v17.i32.3665. PMC 3181451. PMID 21990947.
- ^ Greer FR, Sicherer SH, Burks AW (January 2008). "Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas". Pediatrics. 121 (1): 183–191. doi:10.1542/peds.2007-3022. PMID 18166574.
- ^ Chan ES, Abrams EM, Hildebrand KJ, Watson W (12 September 2018). "Early introduction of foods to prevent food allergy". Allergy, Asthma, and Clinical Immunology. 14 (Suppl 2): 57. doi:10.1186/s13223-018-0286-1. PMC 6157280. PMID 30275847.
- ^ Du Toit G, Roberts G, Sayre PH, Bahnson HT, Radulovic S, Santos AF, et al. (February 2015). "Randomized trial of peanut consumption in infants at risk for peanut allergy". The New England Journal of Medicine. 372 (9): 803–813. doi:10.1056/NEJMoa1414850. PMC 4416404. PMID 25705822.
- ^ Sicherer 2006, pp. 151–8
- ^ "Introducing Foods and Allergy Prevention". - Australasian Society of Clinical Immunology and Allergy (ASCIA). Retrieved 1 January 2023.
- ^ a b c d Leonardi S, Pecoraro R, Filippelli M, Miraglia del Giudice M, Marseglia G, Salpietro C, et al. (2014). "Allergic reactions to foods by inhalation in children". Allergy and Asthma Proceedings. 35 (4): 288–294. doi:10.2500/aap.2014.35.3755. PMID 24992548.
- ^ James JM, Crespo JF (June 2007). "Allergic reactions to foods by inhalation". Current Allergy and Asthma Reports. 7 (3): 167–174. doi:10.1007/s11882-007-0017-z. PMID 17448326. S2CID 11974562.
- ^ Vitaliti G, Pavone P, Spataro G, Giunta L, Guglielmo F, Falsaperla R (2015). "Legumes steam allergy in childhood: Update of the reported cases". Allergologia et Immunopathologia. 43 (2): 196–202. doi:10.1016/j.aller.2013.09.009. PMID 24411097.
- ^ "European Food Allergy and Anaphalaxis Public Declaration". the European Academy of Allergy and Clinical Immunology (EAACI). Archived from the original on 15 December 2013. Retrieved 10 December 2013.
- ^ Sicherer 2006, p. 133
- ^ Sicherer 2006, p. 131
- ^ Sicherer 2006, p. 134
- ^ Persaud, Y; Memon, RJ; Savliwala, MN (2023), "Allergy Immunotherapy", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30570988, retrieved 22 December 2023
- ^ Allison Aubrey (26 February 2024). "Asthma drug can help reduce allergic reactions for those with severe food allergies". NPR.
- ^ Zuberbier T, Wood RA, Bindslev-Jensen C, Fiocchi A, Chinthrajah RS, Worm M, Deschildre A, Fernandez-Rivas M, Santos AF, Jaumont X, Tassinari P (April 2023). "Omalizumab in IgE-Mediated Food Allergy: A Systematic Review and Meta-Analysis". J Allergy Clin Immunol Pract. 11 (4): 1134–46. doi:10.1016/j.jaip.2022.11.036. PMID 36529441.
- ^ a b c d e Loh W, Tang ML (September 2018). "The Epidemiology of Food Allergy in the Global Context". International Journal of Environmental Research and Public Health. 15 (9): 2043. doi:10.3390/ijerph15092043. PMC 6163515. PMID 30231558.
- ^ Lopez CM, Yarrarapu SN, Mendez MD (2022). Food Allergies. Treasure Island (FL): StatPearls Publishing. PMID 29489188.
{{cite book}}:|work=ignored (help) - ^ a b c Iweala OI, Nagler CR (April 2019). "The Microbiome and Food Allergy". Annual Review of Immunology. 37 (1): 377–403. doi:10.1146/annurev-immunol-042718-041621. PMC 10445337. PMID 31026410. S2CID 135423279.
- ^ Warren CM, Jiang J, Gupta RS (February 2020). "Epidemiology and Burden of Food Allergy". Current Allergy and Asthma Reports. 20 (2): 6. doi:10.1007/s11882-020-0898-7. PMC 7883751. PMID 32067114.
- ^ Urisu A, Ebisawa M, Ito K, Aihara Y, Ito S, Mayumi M, et al. (Japanese Society of Allergology, Japanese Society of Pediatric Allergy and Clinical Immunology, Committee for Japanese Pediatric Guideline for Food Allergy) (September 2014). "Japanese Guideline for Food Allergy 2014". Allergology International. 63 (3): 399–419. doi:10.2332/allergolint.14-RAI-0770. PMID 25178179.
- ^ "Rice Allergy". HealthCentersOnline. 2006. p. 2. Archived from the original on 23 May 2006. Retrieved 26 October 2006.
- ^ Lucendo AJ, Arias A, Gonzalez-Cervera J, Mota-Huertas T, Yague-Compadre JL. Tolerance of a cow's milk-based hydrolyzed formula in patients with eosinophilic esophagitis triggered by milk. Allergy; 68:1065–72. Link Archived 2016-11-28 at the Wayback Machine
- ^ "What Are Food Allergies? Food Allergy Summary". Asthma and Allergy Foundation of America. 28 March 2007. Archived from the original on 27 October 2007. Retrieved 6 April 2007.
- ^ Sampson HA (May 2004). "Update on food allergy". The Journal of Allergy and Clinical Immunology. 113 (5): 805–19, quiz 820. doi:10.1016/j.jaci.2004.03.014. PMID 15131561.
- ^ Sicherer SH, Sampson HA (February 2006). "9. Food allergy". The Journal of Allergy and Clinical Immunology. 117 (2 Suppl Mini-Primer): S470–S475. doi:10.1016/j.jaci.2005.05.048. PMID 16455349.
- ^ "Food Allergy Media Q&A" (PDF). Food Allergy & Anaphylaxis Network. 26 May 2010. Archived from the original (PDF) on 30 December 2010. Retrieved 25 March 2011.
- ^ Kagan RS (February 2003). "Food allergy: an overview". Environmental Health Perspectives. 111 (2): 223–225. doi:10.1289/ehp.5702. PMC 1241355. PMID 12573910.
- ^ Branum AM, Lukacs SL (October 2008). "Food allergy among U.S. children: trends in prevalence and hospitalizations". NCHS Data Brief (10): 1–8. PMID 19389315.
- ^ Ben-Shoshan M, Turnbull E, Clarke A (August 2012). "Food allergy: temporal trends and determinants". Current Allergy and Asthma Reports. 12 (4): 346–372. doi:10.1007/s11882-012-0274-3. PMID 22723032. S2CID 25143356.
- ^ Question 6: How serious are food allergies? Food Allergen Labeling And Consumer Protection Act of 2004 Questions and Answers, U.S. Food and Drug Administration (2006).
- ^ Ravid NL, Annunziato RA, Ambrose MA, Chuang K, Mullarkey C, Sicherer SH, et al. (March 2015). "Mental health and quality-of-life concerns related to the burden of food allergy". The Psychiatric Clinics of North America. 38 (1): 77–89. doi:10.1016/j.psc.2014.11.004. PMID 25725570.
- ^ Morou Z, Tatsioni A, Dimoliatis ID, Papadopoulos NG (2014). "Health-related quality of life in children with food allergy and their parents: a systematic review of the literature". Journal of Investigational Allergology & Clinical Immunology. 24 (6): 382–395. PMID 25668890.
- ^ a b Lange L (2014). "Quality of life in the setting of anaphylaxis and food allergy". Allergo Journal International. 23 (7): 252–260. doi:10.1007/s40629-014-0029-x. PMC 4479473. PMID 26120535.
- ^ a b van der Velde JL, Dubois AE, Flokstra-de Blok BM (December 2013). "Food allergy and quality of life: what have we learned?". Current Allergy and Asthma Reports. 13 (6): 651–661. doi:10.1007/s11882-013-0391-7. PMID 24122150. S2CID 326837.
- ^ Culinary Institute of America Allergen-free dining oasis comes to the CIA (2017)
- ^ Shah E, Pongracic J (August 2008). "Food-induced anaphylaxis: who, what, why, and where?". Pediatric Annals. 37 (8): 536–541. doi:10.3928/00904481-20080801-06. PMID 18751571.
- ^ a b c d e f g h Center for Food Safety and Applied Nutrition (8 November 2018). "Guidance for Industry: Questions and Answers Regarding Food Allergens (Edition 4)". U.S. Food and Drug Administration. Retrieved 8 September 2019.
- ^ a b c d e f g h i j k l "Common food allergens". Health Canada. 21 June 2005. Retrieved 8 September 2019.
- ^ a b c d e f g h i j k l m n "Allergen labelling for food manufacturers". Food Standards Agency. Retrieved 8 September 2019.
- ^ a b c d e f g h i j k l "Allergen labelling for consumers | Food Standards Australia New Zealand". www.foodstandards.gov.au. Retrieved 5 May 2024.
- ^ a b c d e f g h i j k l m n "REGULATION (EU) No 1169/2011 OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 25 October 2011 on the provision of food information to consumers, amending Regulations (EC) No 1924/2006 and (EC) No 1925/2006 of the European Parliament and of the Council, and repealing Commission Directive 87/250/EEC, Council Directive 90/496/EEC, Commission Directive 1999/10/EC, Directive 2000/13/EC of the European Parliament and of the Council, Commission Directives 2002/67/EC and 2008/5/EC and Commission Regulation (EC) No 608/2004". 25 October 2011.
- ^ "Food Allergy Safety, Treatment, Education, and Research Act of 2021 or the FASTER Act of 2021". Congress.gov. 4 April 2021. Retrieved 12 October 2021.
- ^ a b "Agência Nacional de Vigilância Sanitária Guia sobre Programa de Controle de Alergênicos" (in Portuguese). Agência Nacional de Vigilância Sanitária (ANVISA). 2016. Archived from the original on 29 April 2018. Retrieved 7 April 2018.
- ^ a b c "Food Allergen Labeling and Consumer Protection Act of 2004". FDA. 2 August 2004. Archived from the original on 28 May 2009.
- ^ a b "Food allergen labelling and information requirements under the EU Food Information for Consumers Regulation No. 1169/2011: Technical Guidance" Archived 7 July 2017 at the Wayback Machine (April 2015).
- ^ a b FDA (14 December 2017). "Have Food Allergies? Read the Label". Food and Drug Administration. Retrieved 14 January 2018.
- ^ a b "Food Ingredients of Public Health Concern" (PDF). United States Department of Agriculture. Food Safety and Inspection Service. 7 March 2017. Retrieved 16 February 2018.
- ^ a b "Allergies and Food Safety". United States Department of Agriculture. Food Safety and Inspection Service. 1 December 2016. Retrieved 16 February 2018.
- ^ a b c d e Allen KJ, Turner PJ, Pawankar R, Taylor S, Sicherer S, Lack G, et al. (2014). "Precautionary labelling of foods for allergen content: are we ready for a global framework?". The World Allergy Organization Journal. 7 (1): 10. doi:10.1186/1939-4551-7-10. PMC 4005619. PMID 24791183.
- ^ a b c FDA (18 December 2017). "Food Allergies: What You Need to Know". Food and Drug Administration. Retrieved 12 January 2018.
- ^ "Statement from FDA Commissioner Scott Gottlieb, M.D., on the FDA's new consideration of labeling for sesame allergies". U.S. Food and Drug Administration. 29 October 2018. Retrieved 8 December 2019.
- ^ "FDA Issues Draft Guidance for Industry on Voluntary Disclosure of Sesame When Added as Flavoring or Spice". U.S. Food and Drug Administration. 10 November 2020. Retrieved 11 November 2020.
- ^ "Food Allergy Safety, Treatment, Education, and Research Act of 2021 or the FASTER Act of 2021". Congress.gov. 4 April 2021. Retrieved 5 March 2022.
- ^ Roses JB (2011). "Food allergen law and the Food Allergen Labeling and Consumer Protection Act of 2004: falling short of true protection for food allergy sufferers". Food and Drug Law Journal. 66 (2): 225–42, ii. PMID 24505841.
- ^ FDA (18 July 2006). "Food Allergen Labeling And Consumer Protection Act of 2004 Questions and Answers". Food and Drug Administration. Retrieved 12 March 2018.
- ^ "Allergy and intolerance: guidance for businesses". Archived from the original on 8 December 2014. Retrieved 12 December 2014.
- ^ Shah AV, Serajuddin AT, Mangione RA (May 2018). "Making All Medications Gluten Free". Journal of Pharmaceutical Sciences. 107 (5): 1263–1268. doi:10.1016/j.xphs.2017.12.021. PMID 29287928.
- ^ Mills EN, Valovirta E, Madsen C, Taylor SL, Vieths S, Anklam E, et al. (December 2004). "Information provision for allergic consumers--where are we going with food allergen labelling?". Allergy. 59 (12): 1262–1268. doi:10.1111/j.1398-9995.2004.00720.x. PMID 15507093. S2CID 40395908.
- ^ Taylor SL, Baumert JL (2015). "Worldwide food allergy labeling and detection of allergens in processed foods". Food Allergy: Molecular Basis and Clinical Practice. Chemical Immunology and Allergy. Vol. 101. pp. 227–234. doi:10.1159/000373910. ISBN 978-3-318-02340-4. PMID 26022883.
{{cite book}}:|journal=ignored (help) - ^ a b DunnGalvin A, Chan CH, Crevel R, Grimshaw K, Poms R, Schnadt S, et al. (September 2015). "Precautionary allergen labelling: perspectives from key stakeholder groups". Allergy. 70 (9): 1039–1051. doi:10.1111/all.12614. PMID 25808296. S2CID 18362869.
- ^ Zurzolo GA, de Courten M, Koplin J, Mathai ML, Allen KJ (June 2016). "Is advising food allergic patients to avoid food with precautionary allergen labelling out of date?". Current Opinion in Allergy and Clinical Immunology. 16 (3): 272–277. doi:10.1097/ACI.0000000000000262. PMID 26981748. S2CID 21326926.
- ^ Athas E (28 January 2019). "Which Allergens Are in Your Food? You Can't Always Tell From the Labels". The New York Times. ISSN 0362-4331. Retrieved 9 December 2019.
- ^ Allen KJ, Remington BC, Baumert JL, Crevel RW, Houben GF, Brooke-Taylor S, et al. (January 2014). "Allergen reference doses for precautionary labeling (VITAL 2.0): clinical implications". The Journal of Allergy and Clinical Immunology. 133 (1): 156–164. doi:10.1016/j.jaci.2013.06.042. PMID 23987796.
- ^ Taylor SL, Baumert JL, Kruizinga AG, Remington BC, Crevel RW, Brooke-Taylor S, et al. (January 2014). "Establishment of Reference Doses for residues of allergenic foods: report of the VITAL Expert Panel". Food and Chemical Toxicology. 63: 9–17. doi:10.1016/j.fct.2013.10.032. PMID 24184597.
- ^ The VITAL Program Allergen Bureau, Australia and New Zealand.
- ^ Popping B, Diaz-Amigo C (January 2018). "European Regulations for Labeling Requirements for Food Allergens and Substances Causing Intolerances: History and Future". Journal of AOAC International. 101 (1): 2–7. doi:10.5740/jaoacint.17-0381. PMID 29202901.
- ^ Nicolia A, Manzo A, Veronesi F, Rosellini D (March 2014). "An overview of the last 10 years of genetically engineered crop safety research" (PDF). Critical Reviews in Biotechnology. 34 (1): 77–88. doi:10.3109/07388551.2013.823595. PMID 24041244. S2CID 9836802. Archived from the original (PDF) on 17 September 2016. Retrieved 2 January 2019.
- ^ "State of Food and Agriculture 2003–2004. Agricultural Biotechnology: Meeting the Needs of the Poor. Health and environmental impacts of transgenic crops". Food and Agriculture Organization of the United Nations. Retrieved 8 February 2016.
- ^ National Academies Of Sciences, Engineering; Division on Earth Life Studies; Board on Agriculture Natural Resources; Committee on Genetically Engineered Crops: Past Experience Future Prospects (2016). Genetically Engineered Crops: Experiences and Prospects. The National Academies of Sciences, Engineering, and Medicine (US). p. 149. doi:10.17226/23395. ISBN 978-0-309-43738-7. PMID 28230933. Retrieved 19 May 2016.
- ^ a b c d Dunn SE, Vicini JL, Glenn KC, Fleischer DM, Greenhawt MJ (September 2017). "The allergenicity of genetically modified foods from genetically engineered crops: A narrative and systematic review". Annals of Allergy, Asthma & Immunology. 119 (3): 214–222.e3. doi:10.1016/j.anai.2017.07.010. PMID 28890018.
- ^ a b c Lee TH, Ho HK, Leung TF (June 2017). "Genetically modified foods and allergy". Hong Kong Medical Journal = Xianggang Yi Xue Za Zhi. 23 (3): 291–295. doi:10.12809/hkmj166189. hdl:10722/243781. PMID 28473652.
- ^ a b Selb R, Wal JM, Moreno FJ, Lovik M, Mills C, Hoffmann-Sommergruber K, Fernandez A (March 2017). "Assessment of endogenous allergenicity of genetically modified plants exemplified by soybean - Where do we stand?". Food and Chemical Toxicology. 101: 139–148. doi:10.1016/j.fct.2017.01.014. hdl:10261/150576. PMID 28111299.
- ^ Bucchini L, Goldman LR (January 2002). "Starlink corn: a risk analysis". Environmental Health Perspectives. 110 (1): 5–13. doi:10.1289/ehp.021105. PMC 1240687. PMID 11781159.
- ^ Wen H, Kwon J (2016). "Food Allergy Risk Communication in Restaurants" (PDF). Food Protection Trends. 35 (5): 372–383.
- ^ a b c d Hadley C (November 2006). "Food allergies on the rise? Determining the prevalence of food allergies, and how quickly it is increasing, is the first step in tackling the problem". EMBO Reports. 7 (11): 1080–1083. doi:10.1038/sj.embor.7400846. PMC 1679775. PMID 17077863.
- ^ Fong AT, Katelaris CH, Wainstein B (July 2017). "Bullying and quality of life in children and adolescents with food allergy". Journal of Paediatrics and Child Health. 53 (7): 630–635. doi:10.1111/jpc.13570. PMID 28608485. S2CID 9719096.
- ^ "The Social Impact of Food Allergies". HuffPost. 23 December 2013. Retrieved 1 January 2023.
- ^ a b Abo MM, Slater MD, Jain P (July 2017). "Using Health Conditions for Laughs and Health Policy Support: The Case of Food Allergies". Health Communication. 32 (7): 803–811. doi:10.1080/10410236.2016.1172292. PMID 27436408. S2CID 3858223.
- ^ a b "How the Media Portrays Food Allergies". Food Allergy Research and Education (FARE). Retrieved 12 September 2022.
- ^ Sony Apologizes for 'Peter Rabbit' Movie's Allergy Scene New York Times, Jacey Fortrin, Feb 12, 2018.
- ^ Wesemann DR, Nagler CR (April 2016). "The Microbiome, Timing, and Barrier Function in the Context of Allergic Disease". Immunity. 44 (4): 728–738. doi:10.1016/j.immuni.2016.02.002. PMC 4869964. PMID 27096316.
- ^ Nowak-Węgrzyn A, Sampson HA (March 2011). "Future therapies for food allergies". The Journal of Allergy and Clinical Immunology. 127 (3): 558–73, quiz 574–5. doi:10.1016/j.jaci.2010.12.1098. PMC 3066474. PMID 21277625.
- ^ a b Best KP, Gold M, Kennedy D, Martin J, Makrides M (January 2016). "Omega-3 long-chain PUFA intake during pregnancy and allergic disease outcomes in the offspring: a systematic review and meta-analysis of observational studies and randomized controlled trials". The American Journal of Clinical Nutrition. 103 (1): 128–143. doi:10.3945/ajcn.115.111104. PMID 26675770.
- ^ a b c Gunaratne AW, Makrides M, Collins CT (July 2015). "Maternal prenatal and/or postnatal n-3 long chain polyunsaturated fatty acids (LCPUFA) supplementation for preventing allergies in early childhood". The Cochrane Database of Systematic Reviews. 2015 (7): CD010085. doi:10.1002/14651858.CD010085.pub2. PMC 8783748. PMID 26197477.
- ^ Waidyatillake NT, Dharmage SC, Allen KJ, Lodge CJ, Simpson JA, Bowatte G, et al. (February 2018). "Association of breast milk fatty acids with allergic disease outcomes-A systematic review". Allergy. 73 (2): 295–312. doi:10.1111/all.13300. PMID 28869762.
- ^ Schindler T, Sinn JK, Osborn DA (October 2016). "Polyunsaturated fatty acid supplementation in infancy for the prevention of allergy". The Cochrane Database of Systematic Reviews. 2016 (10): CD010112. doi:10.1002/14651858.CD010112.pub2. PMC 6464137. PMID 27788565.
- ^ Chang YS, Trivedi MK, Jha A, Lin YF, Dimaano L, García-Romero MT (March 2016). "Synbiotics for Prevention and Treatment of Atopic Dermatitis: A Meta-analysis of Randomized Clinical Trials". JAMA Pediatrics. 170 (3): 236–242. doi:10.1001/jamapediatrics.2015.3943. PMID 26810481.
- ^ a b Cuello-Garcia CA, Brożek JL, Fiocchi A, Pawankar R, Yepes-Nuñez JJ, Terracciano L, et al. (October 2015). "Probiotics for the prevention of allergy: A systematic review and meta-analysis of randomized controlled trials". The Journal of Allergy and Clinical Immunology. 136 (4): 952–961. doi:10.1016/j.jaci.2015.04.031. PMID 26044853.
- ^ a b Osborn DA, Sinn JK (March 2013). "Prebiotics in infants for prevention of allergy". The Cochrane Database of Systematic Reviews. 2013 (3): CD006474. doi:10.1002/14651858.CD006474.pub3. PMID 23543544.
- ^ Zuccotti G, Meneghin F, Aceti A, Barone G, Callegari ML, Di Mauro A, et al. (November 2015). "Probiotics for prevention of atopic diseases in infants: systematic review and meta-analysis". Allergy. 70 (11): 1356–1371. doi:10.1111/all.12700. PMID 26198702.
- ^ Zhang GQ, Hu HJ, Liu CY, Zhang Q, Shakya S, Li ZY (February 2016). "Probiotics for Prevention of Atopy and Food Hypersensitivity in Early Childhood: A PRISMA-Compliant Systematic Review and Meta-Analysis of Randomized Controlled Trials". Medicine. 95 (8): e2562. doi:10.1097/MD.0000000000002562. PMC 4778993. PMID 26937896.
- ^ de Silva D, Geromi M, Panesar SS, Muraro A, Werfel T, Hoffmann-Sommergruber K, et al. (February 2014). "Acute and long-term management of food allergy: systematic review". Allergy. 69 (2): 159–167. doi:10.1111/all.12314. PMID 24215577. S2CID 206999857.
- Notes
- Nester EW, Anderson DG, Roberts Jr CE, Nester MT (2009). "Immunologic Disorders". Microbiology: A Human Perspective (6th ed.). New York: McGraw-Hill. pp. 414–428.
- Sicherer SH (2006). Understanding and Managing Your Child's Food Allergy. Baltimore: Johns Hopkins University Press.
External links
[edit]- Food Allergy, Merck Manual
- "Food Allergies and Intolerances Resource List for Consumers" (PDF). Food and Nutrition Information Center, National Agricultural Library. December 2010. Archived from the original (PDF) on 6 August 2011. Retrieved 15 August 2011. – a collection of resources on the topic of food allergies and intolerances
- "Food Allergy". MedlinePlus. U.S. National Library of Medicine.
