Obstetrics
This article may be too technical for most readers to understand. (September 2010) |
| Occupation | |
|---|---|
| Names |
|
Occupation type | Specialty |
Activity sectors | Medicine, surgery |
| Description | |
Education required |
|
Fields of employment | Hospitals, clinics |
Obstetrics is the field of study concentrated on pregnancy, childbirth and the postpartum period.[1] As a medical specialty, obstetrics is combined with gynecology under the discipline known as obstetrics and gynecology (OB/GYN), which is a surgical field.[2]
Main areas
[edit]Prenatal care
[edit]Prenatal care is important in screening for various complications of pregnancy.[3] This includes routine office visits with physical exams and routine lab tests along with telehealth care for women with low-risk pregnancies:[4]
-
3D ultrasound of 3-inch (76 mm) fetus (about 14 weeks gestational age)
-
Fetus at 17 weeks
-
Fetus at 20 weeks
First trimester
[edit]Routine tests in the first trimester of pregnancy generally include:
- Complete blood count
- Blood type
- Rh-negative antenatal patients should receive RhoGAM at 28 weeks to prevent Rh disease.
- Indirect Coombs test (AGT) to assess risk of hemolytic disease of the newborn[5]
- Rapid plasma reagin test to screen for syphilis
- Rubella antibody screen[6]
- HBsAg test to screen for hepatitis B[7]
- Testing for chlamydia (and gonorrhea when indicated[8]
- Mantoux test for tuberculosis[9]
- Urinalysis and culture[10]
- HIV screen
Genetic screening for Down syndrome (trisomy 21) and Edwards syndrome (trisomy 18), the national standard in the United States, is rapidly evolving away from the AFP-quad screen, done typically in the second trimester at 16–18 weeks.[11] The newer integrated screen (formerly called F.A.S.T.E.R for First And Second Trimester Early Results) can be done at 10 plus weeks to 13 plus weeks with an ultrasound of the fetal neck (thicker nuchal skin correlates with higher risk of Down syndrome being present) and two chemicals (analytes), pregnancy-associated plasma protein A and human chorionic gonadotropin (pregnancy hormone level itself[12]). It gives an accurate risk profile very early. A second blood screen at 15 to 20 weeks refines the risk more accurately.[13] The cost is higher than an "AFP-quad" screen due to the ultrasound and second blood test, but it is quoted to have a 93% pick up rate as opposed to 88% for the standard AFP/QS. This is an evolving standard of care in the United States.[14][15][16]
Second trimester
[edit]- MSAFP/quad. screen (four simultaneous blood tests) (maternal serum AFP, inhibin A, estriol, and βHCG) – elevations, low numbers or odd patterns correlate with neural tube defect risk and increased risks of trisomy 18 or trisomy 21[17]
- Ultrasound either abdominal or transvaginal to assess cervix, placenta, fluid and baby[18]
- Amniocentesis is the national standard for women over 35 or who reach 35 by mid pregnancy or who are at increased risk by family history or prior birth history.[16]
Third trimester
[edit]- Hematocrit (if low, the mother receives iron supplements)[19]
- Group B Streptococcus screen. If positive, the woman receives IV penicillin or ampicillin while in labor—or, if she is allergic to penicillin, an alternative therapy, such as IV clindamycin or IV vancomycin.[16]
- Glucose loading test (GLT) – screens for gestational diabetes; if > 140 mg/dL, a glucose tolerance test (GTT) is administered; a fasting glucose > 105 mg/dL suggests gestational diabetes.[20]
Most doctors do a sugar load in a drink form of 50 grams of glucose in cola, lime or orange and draw blood an hour later (plus or minus 5 minutes). The standard modified criteria have been lowered to 135 since the late 1980s.[21]

Fetal assessments
[edit]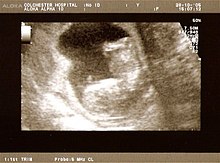
Obstetric ultrasonography is routinely used for dating the gestational age of a pregnancy from the size of the fetus, determine the number of fetuses and placentae, evaluate for an ectopic pregnancy and first trimester bleeding, the most accurate dating being in first trimester before the growth of the foetus has been significantly influenced by other factors.[22] Ultrasound is also used for detecting congenital anomalies (or other foetal anomalies) and determining the biophysical profiles (BPP), which are generally easier to detect in the second trimester when the foetal structures are larger and more developed.[23]
X-rays and computerized tomography (CT) are not used, especially in the first trimester, due to the ionizing radiation, which has teratogenic effects on the foetus.[24] No effects of magnetic resonance imaging (MRI) on the foetus have been demonstrated,[25] but this technique is too expensive for routine observation. Instead, obstetric ultrasonography is the imaging method of choice in the first trimester and throughout the pregnancy, because it emits no radiation, is portable, and allows for realtime imaging.[26]
The safety of frequent ultrasound scanning has not been confirmed. Despite this, increasing numbers of women are choosing to have additional scans for no medical purpose, such as gender scans, 3D and 4D scans.[27] A normal gestation would reveal a gestational sac, yolk sac, and fetal pole.[28]
The gestational age can be assessed by evaluating the mean gestational sac diameter (MGD) before week 6, and the crown-rump length after week 6. Multiple gestation is evaluated by the number of placentae and amniotic sacs present.[29]
Other tools used for assessment include:
- Fetal screening is used to help assess the viability of the fetus, as well as congenital abnormalities.[30]
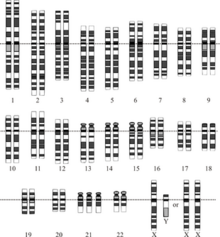
- Fetal karyotype can be used for the screening of genetic diseases. This can be obtained via amniocentesis or chorionic villus sampling (CVS[31])
- Foetal haematocrit for the assessment of foetal anemia, Rh isoimmunization, or hydrops can be determined by percutaneous umbilical blood sampling (PUBS), which is done by placing a needle through the abdomen into the uterus and taking a portion of the umbilical cord.[32]
- Fetal lung maturity is associated with how much surfactant the fetus is producing. Reduced production of surfactant indicates decreased lung maturity and is a high risk factor for infant respiratory distress syndrome.[33] Typically a lecithin:sphingomyelin ratio greater than 1.5 is associated with increased lung maturity.
- Nonstress test (NST) for fetal heart rate[34]
- Oxytocin challenge test
Diseases in pregnancy
[edit]A pregnant woman may have a pre-existing disease, that may become worse or become a risk to the pregnancy, or to postnatal development of the offspring[35]
- Diabetes mellitus and pregnancy deals with the interactions of diabetes mellitus (not restricted to gestational diabetes) and pregnancy.[36] Risks for the child include miscarriage, growth restriction, growth acceleration, foetal obesity (macrosomia), polyhydramnios and birth defects.
- Lupus and pregnancy confers an increased rate of foetal death in utero and spontaneous abortion (miscarriage), as well as of neonatal lupus.[37]
- Thyroid disease in pregnancy can, if uncorrected, cause adverse effects on foetal and maternal well-being.[38] The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child.[39] Demand for thyroid hormones is increased during pregnancy, and may cause a previously unnoticed thyroid disorder to worsen.[citation needed]
- Hypercoagulability in pregnancy is the propensity of pregnant women to develop thrombosis (blood [40] clots). Pregnancy itself is a factor of hypercoagulability (pregnancy-induced hypercoagulability), as a physiologically adaptive mechanism to prevent post partum bleeding.[41] However, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.[41]
- Hyperemesis gravidarum in pregnancy occurs due to extreme, persistent nausea and vomiting during pregnancy.[42] If untreated, can lead to dehydration, weight loss, and electrolyte imbalances. Most women develop nausea and vomiting during the first trimester.[43] The cause of hyperemesis gravidarum is not known. However, it is believed to be caused by a rapidly rising blood level of a hormone, human chorionic gonadotropin (HCG), which is released by the placenta.
- Preeclampsia is a condition that causes high blood pressure during pregnancy. If left untreated, it can be life-threatening.[44] In pregnant women, preeclampsia may occur after 20 weeks of pregnancy, often in women who have no history of high blood pressure. Symptoms of preeclampsia may include severe headache, vision changes and pain under the ribs.[45] However, in some women, symptoms may not occur, until they go for a routine prenatal visit.[46]
Induction and labour
[edit]Induction is a method of artificially or prematurely stimulating labour in a woman.[47] Reasons to induce can include pre-eclampsia, foetal distress, placental malfunction, intrauterine growth retardation and failure to progress through labour increasing the risk of infection and foetal distresses.[48]
Induction may be achieved via several methods:
- Disturbance of cervical membranes[49]
- Pessary of Prostin cream, prostaglandin E2[50]
- Intravaginal or oral administration of misoprostol[51]
- Cervical insertion of a 30-mL Foley catheter[52]
- Rupturing the amniotic membranes[53]
- Intravenous infusion of synthetic oxytocin (Pitocin or Syntocinon)[54]
During labour, the obstetrician carries out the following tasks:
- Monitor the progress of labour, by reviewing the nursing chart, performing vaginal examination, and assessing the trace produced by a foetal monitoring device (the cardiotocograph)[55]
- Provide pain relief, either by nitrous oxide, opiates, or by epidural anaesthesia done by anaesthestists, an anaesthesiologist, or a nurse anaesthetist.[56]
- Caesarean section, if there is an associated risk with vaginal delivery, as such foetal or maternal compromise.[57]
Complications and emergencies
[edit]The main emergencies include:
- Ectopic pregnancy is when an embryo implants in the uterine (fallopian) tube or (rarely) on the ovary or inside the peritoneal cavity. This may cause massive internal bleeding.[58]
- Pre-eclampsia is a disease defined by a combination of signs and symptoms that are related to maternal hypertension.[59] The cause is unknown, and markers are being sought to predict its development from the earliest stages of pregnancy.[60] Some unknown factors cause vascular damage in the endothelium, causing hypertension.[61] If severe, it progresses to eclampsia, where seizures occur, which can be fatal.[62] Preeclamptic patients with the HELLP syndrome show liver failure and disseminated intravascular coagulation (DIC).[63] The only treatment is to deliver the foetus. Women may still develop pre-eclampsia following delivery.[64]
- Placental abruption is where the placenta detaches from the uterus and the woman and foetus can bleed to death if not managed appropriately.[65]
- Foetal distress where the foetus is getting compromised in the uterine environment.[66]
- Shoulder dystocia where one of the foetus' shoulders becomes stuck during vaginal birth. There are many risk factors, including macrosmic (large) foetus, but many are also unexplained.[67]
- Uterine rupture can occur during obstructed labour and endanger foetal and maternal life.[68]
- Prolapsed cord can only happen after the membranes have ruptured.[69] The umbilical cord delivers before the presenting part of the foetus. If the foetus is not delivered within minutes, or the pressure taken off the cord, the foetus dies.[70]
- Obstetrical hemorrhage may be due to a number of factors such as placenta previa, uterine rupture or tears, uterine atony, retained placenta or placental fragments, or bleeding disorders.[71]
- Puerperal sepsis is an ascending infection of the genital tract.[72] It may happen during or after labour. Signs to look out for include signs of infection (pyrexia or hypothermia, raised heart rate and respiratory rate, reduced blood pressure), and abdominal pain, offensive lochia (blood loss) increased lochia, clots, diarrhea and vomiting.[citation needed]
Postpartum period
[edit]The World Health Organization makes a distinction between the use of postpartum care when it concerns the care of the mother after giving birth, and postnatal care when the care of the newborn is concerned.[73] Postpartum care is provided to the mother following childbirth.
A woman in the Western world who gives birth in a hospital may leave the hospital as soon as she is medically stable, and chooses to leave, which can be as early as a few hours later, but usually averages a stay of one or two days; the average postnatal stay following delivery by caesarean section is three to four days.[74]
During this time the mother is monitored for bleeding, bowel and bladder function, and baby care. The infant's health is also monitored.[75]
Veterinary obstetrics
[edit]History
[edit]
Prior to the 18th century, caring for pregnant women in Europe was confined exclusively to women, and rigorously excluded men.[76] The expectant mother would invite close female friends and family members to her home to keep her company during childbirth.[77]: 96–98 Skilled midwives managed all aspects of the labour and delivery.[78] The presence of physicians and surgeons was very rare and only occurred if a serious complication had taken place and the midwife had exhausted all measures at her disposal.[79] Calling a surgeon was very much a last resort and having men deliver women in this era was seen as offending female modesty.[80]: 1050–1051 [81]
Before the 18th century
[edit]Prior to the 18th and 19th centuries, midwifery was well established but obstetrics was not recognized as a specific medical specialty. However, the subject matter and interest in the female reproductive system and sexual practice can be traced back to Ancient Egypt[82]: 122 and Ancient Greece.[83]: 11 Soranus of Ephesus sometimes is called the most important figure in ancient gynecology.[79] Living in the late first century AD and early second century, he studied anatomy and had opinions and techniques on abortion, contraception – most notably coitus interruptus – and birth complications. After his death, techniques and works of gynecology declined; very little of his works were recorded and survived to the late 18th century when gynecology and obstetrics reemerged as a medical specialism.[82]: 123
18th century
[edit]The 18th century marked the beginning of many advances in European midwifery, based on better knowledge of the physiology of pregnancy and labour.[84] By the end of the century, medical professionals began to understand the anatomy of the uterus and the physiological changes that take place during labour.[85] The introduction of forceps in childbirth also took place at this time. All these medical advances in obstetrics were a lever for the introduction of men into an arena previously managed and run by women – midwifery.[80]: 1051–1052
The addition of the male-midwife (or man-midwife) is historically a significant change to the profession of obstetrics.[86] In the 18th century medical men began to train in area of childbirth and believed with their advanced knowledge in anatomy that childbirth could be improved.[87] In France these male-midwives were referred to as accoucheurs, a title later used all over Europe. The founding of lying-in hospitals also contributed to the medicalization and male-dominance of obstetrics.[88] These early maternity hospitals were establishments where women would come to have their babies delivered, as opposed to the practice since time immemorial of the midwife attending the home of the woman in labour.[89] This institution provided male-midwives with endless patients to practice their techniques on and was a way for these men to demonstrate their knowledge.[90]
Many midwives of the time bitterly opposed the involvement of men in childbirth. Some male practitioners also opposed the involvement of medical men like themselves in midwifery and even went as far as to say that male-midwives only undertook midwifery solely for perverse erotic satisfaction. The accoucheurs argued that their involvement in midwifery was to improve the process of childbirth. These men also believed that obstetrics would forge ahead and continue to strengthen.[80]: 1050–1051
19th century
[edit]18th-century physicians expected that obstetrics would continue to grow, but the opposite happened. Obstetrics entered a stage of stagnation in the 19th century, which lasted until about the 1880s.[77]: 96–98 The central explanation for the lack of advancement during this time was the rejection of obstetrics by the medical community.[91] The 19th century marked an era of medical reform in Europe and increased regulation over the profession. Major European institutions such as The College of Physicians and Surgeons[where?] considered delivering babies ungentlemanly work and refused to have anything to do with childbirth as a whole. Even when Medical Act 1858 was introduced, which stated that medical students could qualify as doctors, midwifery was entirely ignored.[92] This made it nearly impossible to pursue an education in midwifery and also have the recognition of being a doctor or surgeon. Obstetrics was pushed to the side.[80]: 1053–1055
By the late 19th century, the foundation of modern-day obstetrics and midwifery began developing. Delivery of babies by doctors became popular and readily accepted, but midwives continued to play a role in childbirth.[87] Midwifery also changed during this era due to increased regulation and the eventual need for midwives to become certified.[93] Many European countries by the late 19th century were monitoring the training of midwives and issued certification based on competency. Midwives were no longer uneducated in the formal sense.[94]
As midwifery began to develop, so did the profession of obstetrics near the end of the century.[95] Childbirth was no longer unjustifiably despised by the medical community as it once had been at the beginning of the century. But obstetrics was underdeveloped compared to other medical specialities. Many male physicians would deliver children but very few would have referred to themselves as obstetricians. The end of the 19th century did mark a significant accomplishment in the profession with the advancements in asepsis and anaesthesia, which paved the way for the mainstream introduction and later success of the Caesarean section.[94][96]
Before the 1880s mortality rates in lying-hospitals would reach unacceptably high levels and became an area of public concern. Much of these maternal deaths were due to puerperal fever, then known as childbed fever. In the 1800s Ignaz Semmelweis noticed that women giving birth at home had a much lower incidence of childbed fever than those giving birth by physicians in lying-hospitals. His investigation discovered that washing hands with an antiseptic solution before a delivery reduced childbed fever fatalities by 90%.[97] So it was concluded that it was physicians who had been spreading disease from one labouring mother to the next. Despite the publication of this information, doctors still would not wash. It was not until the 20th century when advancements in aseptic technique and the understanding of disease would play a significant role in the decrease of maternal mortality rates among many populations.[citation needed]
History of obstetrics in America
[edit]The development of obstetrics as a practice for accredited doctors happened at the turn of the 18th century and thus was very differently developed in Europe and in the Americas due to the independence of many countries in the Americas from European powers. "Unlike in Europe and the British Isles, where midwifery laws were national, in America, midwifery laws were local and varied widely".[98]
Gynaecology and Obstetrics gained attention in the American medical field at the end of the nineteenth century through the development of such procedures as the ovariotomy.[99] These procedures then were shared with European surgeons who replicated the surgeries. This was a period when antiseptic, aseptic or anaesthetic measures were just being introduced to surgical and observational procedures and without these procedures surgeries were dangerous and often fatal.[100] Following are two surgeons noted for their contributions to these fields include Ephraim McDowell and J. Marion Sims.[101]
Ephraim McDowell developed a surgical practice in 1795 and performed the first ovariotomy in 1809 on a 47-year-old widow who then lived on for 31 more years.[102] He had attempted to share this with John Bell whom he had practiced under who had retired to Italy. Bell was said to have died without seeing the document but it was published by an associate in Extractions of Diseased Ovaria in 1825.[103] By the mid-century the surgery was both successfully and unsuccessfully being performed. Pennsylvanian surgeons the Attlee brothers made this procedure very routine for a total of 465 surgeries – John Attlee performed 64 successfully of 78 while his brother William reported 387 – between the years of 1843 and 1883.[104] By the middle of the nineteenth century this procedure was successfully performed in Europe by English surgeons Sir Spencer Wells and Charles Clay as well as French surgeons Eugène Koeberlé, Auguste Nélaton and Jules Péan.[82]: 125
J. Marion Sims was the surgeon responsible for being the first treating a vesicovaginal fistula[82]: 125 – a condition linked to many caused mainly by prolonged pressing of the foetus against the pelvis or other causes such as rape, hysterectomy, or other operations – and also having been doctor to many European royals and the 20th President of the United States James A. Garfield after he had been shot. Sims does have a controversial medical past. Under the beliefs at the time about pain and the prejudice towards African people, he had practiced his surgical skills and developed skills on slaves.[105] These women were the first patients of modern gynecology. One of the women he operated on was named Anarcha Westcott, the woman he first treated for a fistula.[105]
Historical role of gender
[edit]Women and men inhabited very different roles in natal care up to the 18th century.[106] The role of a physician was exclusively held by men who went to university, an overly male institution, who would theorize anatomy and the process of reproduction based on theological teaching and philosophy. Many beliefs about the female body and menstruation in the 17th and 18th centuries were inaccurate; clearly resulting from the lack of literature about the practice.[82]: 123–125 Many of the theories of what caused menstruation prevailed from Hippocratic philosophy.[83]: 16 Midwives, meaning "with woman", were those who assisted in the birth and care of both born and unborn children, a position historically held mainly by women.[107]
During the birth of a child, men were rarely present. Women from the neighbourhood or family would join in on the process of birth and assist in many different ways.[108] The one position where men would help with the birth of a child would be in the sitting position, usually when performed on the side of a bed to support the mother.[77]: 130
Men entered the field of obstetrics in the nineteenth century, resulting in a change of focus within the profession.[109] Gynecology developed as a new and separate field of study from obstetrics, focusing on the curing of illness and indispositions of female sexual organs,[110] encompassing conditions such as menopause, uterine and cervical problems, and tissue damage as a result of childbirth.[111]
See also
[edit]- Henry Jacques Garrigues, who introduced antiseptic obstetrics to North America
- Maternal-fetal medicine
- Obstetrical nursing
References
[edit]- ^ "What Is an Obstetrician? What They Do & When To See One". Cleveland Clinic. Retrieved 2022-04-29.
- ^ "Obstetrics and Gynecology Specialty Description". American Medical Association. Retrieved 24 October 2020.
- ^ Tulchinsky TH, Varavikova EA (March 2014). "Chapter 6 - Family Health". The new public health (Third ed.). Academic Press. pp. 311–379. doi:10.1016/B978-0-12-415766-8.00006-9. ISBN 978-0-12-415766-8.
- ^ Cantor, Amy G.; Jungbauer, Rebecca M.; Totten, Annette M.; Tilden, Ellen L.; Holmes, Rebecca; Ahmed, Azrah; Wagner, Jesse; Hermesch, Amy C.; McDonagh, Marian S. (2022). "Telehealth Strategies for the Delivery of Maternal Health Care: A Rapid Review". Annals of Internal Medicine. 175 (9): 1285–1297. doi:10.7326/M22-0737. ISSN 0003-4819. PMID 35878405. S2CID 251067668.
- ^ Rath L. "What Is a Coombs Test?". WebMD. Retrieved 2022-04-29.
- ^ Rath L. "Why Do I Need a Rubella Test?". WebMD. Retrieved 2022-04-29.
- ^ Mekaroonkamol P, Hashemi N (2021-04-03). Staros EB (ed.). "Hepatitis B Test: Reference Range, Interpretation, Collection and Panels". Medscape.
- ^ Fontenot HB, George ER (2014). "Sexually transmitted infections in pregnancy". Nursing for Women's Health. 18 (1): 67–72. doi:10.1111/1751-486X.12095. PMID 24548498.
- ^ CDCTB (2020-12-16). "Tuberculosis (TB) Fact Sheets- Tuberculin Skin Testing". Centers for Disease Control and Prevention. Retrieved 2022-04-29.
- ^ "Urinalysis: What It Is, Purpose, Types & Results". Cleveland Clinic. Retrieved 2022-04-29.
- ^ Cereda A, Carey JC (October 2012). "The trisomy 18 syndrome". Orphanet Journal of Rare Diseases. 7: 81. doi:10.1186/1750-1172-7-81. PMC 3520824. PMID 23088440.
- ^ Malone FD, Canick JA, Ball RH, Nyberg DA, Comstock CH, Bukowski R, et al. (November 2005). "First-trimester or second-trimester screening, or both, for Down's syndrome". The New England Journal of Medicine. 353 (19): 2001–2011. doi:10.1056/NEJMoa043693. PMID 16282175.
- ^ "Common Tests During Pregnancy". www.hopkinsmedicine.org. 2021-08-08. Retrieved 2022-04-29.
- ^ Carlson LM, Vora NL (June 2017). "Prenatal Diagnosis: Screening and Diagnostic Tools". Obstetrics and Gynecology Clinics of North America. 44 (2): 245–256. doi:10.1016/j.ogc.2017.02.004. PMC 5548328. PMID 28499534.
- ^ Zhang W, Mohammadi T, Sou J, Anis AH (2019). "Cost-effectiveness of prenatal screening and diagnostic strategies for Down syndrome: A microsimulation modeling analysis". PLOS ONE. 14 (12): e0225281. Bibcode:2019PLoSO..1425281Z. doi:10.1371/journal.pone.0225281. PMC 6892535. PMID 31800591.
- ^ a b c "Common Tests During Pregnancy". www.hopkinsmedicine.org. 2021-08-08. Retrieved 2022-04-28.
- ^ "Quad screen - Mayo Clinic". www.mayoclinic.org. Retrieved 2022-04-29.
- ^ "Prenatal Ultrasound Procedure Information". Cleveland Clinic. Retrieved 2022-04-29.
- ^ Uscher J. "Anemia in Pregnancy: Causes, Symptoms, and Treatment". WebMD. Retrieved 2022-04-29.
- ^ "Glucose challenge test - Mayo Clinic". www.mayoclinic.org. Retrieved 2022-04-29.
- ^ "Glucose tolerance test - Mayo Clinic". www.mayoclinic.org. Retrieved 2022-04-29.
- ^ Kansky C, Ramus RM (2021-06-15). Pierce Jr JG (ed.). "Basic Obstetric Ultrasound: Background, Indications, Contraindications". Medscape.
- ^ DeFrancesco V (January 2004). "Perinatology.". Clinical Engineering Handbook. Academic Press. pp. 410–416. doi:10.1016/B978-012226570-9/50102-2. ISBN 978-0-12-226570-9.
- ^ Shaw P, Duncan A, Vouyouka A, Ozsvath K (January 2011). "Radiation exposure and pregnancy". Journal of Vascular Surgery. Radiation Safety in Vascular Surgery. 53 (1 Suppl): 28S–34S. doi:10.1016/j.jvs.2010.05.140. PMID 20869193.
- ^ Alorainy IA, Albadr FB, Abujamea AH (2006). "Attitude towards MRI safety during pregnancy". Annals of Saudi Medicine. 26 (4): 306–309. doi:10.5144/0256-4947.2006.306. PMC 6074503. PMID 16885635.
- ^ Herbst MK, Tafti D, Shanahan MM (2022). "Obstetric Ultrasound". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29261880. Retrieved 2022-04-29.
- ^ Edvardsson K, Small R, Persson M, Lalos A, Mogren I (October 2014). "'Ultrasound is an invaluable third eye, but it can't see everything': a qualitative study with obstetricians in Australia". BMC Pregnancy and Childbirth. 14 (1): 363. doi:10.1186/1471-2393-14-363. PMC 4287579. PMID 25336335.
- ^ Weissleder R, Harisinghani MG, Wittenberg J, Chen JW, eds. (2011). "Obstetric Imaging". Primer of Diagnostic Imagin (5th ed.). St. Louis, Mo.: Mosby. pp. 533–574. doi:10.1016/B978-0-323-06538-2.00010-X. ISBN 978-0-323-06538-2.
- ^ Khan AN, Sabih D, Sabih A (2021-04-26). "Early Pregnancy Loss (Embryonic Demise) Imaging: Practice Essentials, Ultrasonography".
- ^ Marino T (2021-06-14). Ramus RM (ed.). "Prenatal Diagnosis for Congenital Malformations and Genetic Disorders: Practice Essentials, Noninvasive Techniques, Invasive Techniques". Medscape.
- ^ "Chorionic villus sampling - Mayo Clinic". www.mayoclinic.org. Retrieved 2022-04-29.
- ^ Gomella TL, Cunningham MD, Eyal FG, Tuttle DJ (2013). Fetal Assessment (7 ed.). New York, NY: McGraw-Hill Education. Retrieved 2022-04-29.
{{cite book}}:|work=ignored (help) - ^ Jobe AH (January 1984). "Fetal lung maturation and the respiratory distress syndrome.". Fetal Physiology and Medicine (Second ed.). Butterworth-Heinemann. pp. 317–351. doi:10.1016/B978-0-407-00366-8.50016-2. ISBN 978-0-407-00366-8.
- ^ "Nonstress test - Mayo Clinic". www.mayoclinic.org. Retrieved 2022-04-29.
- ^ Dunkin MA. "High-Risk Pregnancies: Symptoms, Doctors, Support, and More". WebMD. Retrieved 2022-04-29.
- ^ Moore T (2022-04-06). Griffing GT (ed.). "Diabetes Mellitus and Pregnancy: Practice Essentials, Gestational Diabetes, Maternal-Fetal Metabolism in Normal Pregnancy". Medscape.
- ^ Khurana R, Wolf RE (2021-10-16). Talavera F, Singh AK (eds.). "Systemic Lupus Erythematosus and Pregnancy: Practice Essentials, Pathophysiology, Epidemiology". Medscape.
- ^ Friel LA. "Thyroid Disorders in Pregnancy - Gynecology and Obstetrics". MSD Manual Professional Edition. Retrieved 2022-04-29.
- ^ Alemu A, Terefe B, Abebe M, Biadgo B (November 2016). "Thyroid hormone dysfunction during pregnancy: A review". International Journal of Reproductive Biomedicine. 14 (11): 677–686. PMC 5153572. PMID 27981252.
- ^ Nichols KM, Henkin S, Creager MA (November 2020). "Venous Thromboembolism Associated With Pregnancy: JACC Focus Seminar". Journal of the American College of Cardiology. 76 (18): 2128–2141. doi:10.1016/j.jacc.2020.06.090. PMID 33121721. S2CID 226205234.
- ^ a b Page 264 in: Gresele P (2008). Platelets in haematologic and cardiovascular disorders: a clinical handbook. Cambridge, UK: Cambridge University Press. ISBN 978-0-521-88115-9.
- ^ "Hyperemesis Gravidarum: Symptoms & Treatment". Cleveland Clinic. Retrieved 2022-04-30.
- ^ "Morning sickness - Symptoms and causes". Mayo Clinic. Retrieved 2022-04-30.
- ^ Gaither K (13 December 2019). "Preeclampsia". WebMD. Retrieved 2022-04-29.
- ^ "Preeclampsia - Symptoms and causes". Mayo Clinic. Retrieved 2022-04-29.
- ^ "4 Common Pregnancy Complications". www.hopkinsmedicine.org. 2021-08-08. Retrieved 2022-04-28.
- ^ Healthdirect Australia (2022-02-08). "Induced labour". www.pregnancybirthbaby.org.au. Retrieved 2022-04-29.
- ^ Surányim A (2000). Prenatal and postnatal evaluation of foetal renal hyperechogenicity in pregnancies complicated with pre-eclampsia and intrauterine growth retardation (Ph.D. thesis). University of Szeged. doi:10.14232/phd.2154.
- ^ Moldenhauer JS. "Prelabor Rupture of the Membranes (PROM) - Women's Health Issues". MSD Manual Consumer Version. Retrieved 2022-04-30.
- ^ "Prostin E2 Vaginal: Uses, Side Effects, Interactions, Pictures, Warnings & Dosing - WebMD". www.webmd.com. Retrieved 2022-04-30.
- ^ Ho PC, Ngai SW, Liu KL, Wong GC, Lee SW (November 1997). "Vaginal misoprostol compared with oral misoprostol in termination of second-trimester pregnancy". Obstetrics and Gynecology. 90 (5): 735–738. doi:10.1016/S0029-7844(97)00419-5. PMID 9351755. S2CID 21261210.
- ^ Adeniji OA, Oladokun A, Olayemi O, Adeniji OI, Odukogbe AA, Ogunbode O, et al. (February 2005). "Pre-induction cervical ripening: transcervical foley catheter versus intravaginal misoprostol". Journal of Obstetrics and Gynaecology. 25 (2): 134–139. doi:10.1080/01443610500040737. PMID 15814391. S2CID 24250115.
- ^ "Premature rupture of membranes". MedlinePlus Medical Encyclopedia. Bethesda (MD): U.S. National Library of Medicine. Retrieved 2022-04-30.
- ^ "Oxytocin 10 IU/ml Solution for infusion - Summary of Product Characteristics (SmPC) - (emc)". www.medicines.org.uk. Retrieved 2022-04-30.
- ^ Prior T, Lees C (2019). "Control and Monitoring of Fetal Growth.". Encyclopedia of Endocrine Diseases. Vol. 5. pp. 1–9. doi:10.1016/B978-0-12-801238-3.65414-4. ISBN 9780128122006. S2CID 81797258.
- ^ Lloyd-Thomas AR (January 1990). "Pain management in paediatric patients". British Journal of Anaesthesia. 64 (1): 85–104. doi:10.1093/bja/64.1.85. PMID 2405898.
- ^ Saint Louis H (2022-04-14). "Cesarean Delivery: Overview, Preparation, Technique". Medscape.
- ^ "Ectopic pregnancy - Symptoms and causes". Mayo Clinic. Retrieved 2022-04-30.
- ^ Lim KH, Steinberg G (2022-04-13). "Preeclampsia: Practice Essentials, Overview, Pathophysiology". Medscape.
- ^ Artal-Mittelmark R. "Stages of Development of the Fetus - Women's Health Issues". MSD Manual Consumer Version. Retrieved 2022-04-30.
- ^ "Hypertension: Causes, symptoms, and treatments". www.medicalnewstoday.com. 2021-11-10. Retrieved 2022-04-30.
- ^ Seppa N (2011-01-20). "Body & brain: Uncontrolled epilepsy can be fatal: Study finds more deaths in adults whose seizures persist". Science News. 179 (3): 8. doi:10.1002/scin.5591790305. ISSN 0036-8423.
- ^ Haram K, Svendsen E, Abildgaard U (February 2009). "The HELLP syndrome: clinical issues and management. A Review". BMC Pregnancy and Childbirth. 9 (1): 8. doi:10.1186/1471-2393-9-8. PMC 2654858. PMID 19245695.
- ^ "Preeclampsia: Symptoms, Causes, Treatments & Prevention". Cleveland Clinic. Retrieved 2022-04-30.
- ^ "Placental Abruption: Symptoms, Causes & Effects On Baby". Cleveland Clinic. Retrieved 2022-04-30.
- ^ Moldenhauer JS. "Fetal Distress - Women's Health Issues". MSD Manual Consumer Version. Retrieved 2022-04-30.
- ^ "Shoulder Dystocia: Signs, Causes, Prevention & Complications". Cleveland Clinic. Retrieved 2022-04-30.
- ^ Astatikie G, Limenih MA, Kebede M (April 2017). "Maternal and fetal outcomes of uterine rupture and factors associated with maternal death secondary to uterine rupture". BMC Pregnancy and Childbirth. 17 (1): 117. doi:10.1186/s12884-017-1302-z. PMC 5389173. PMID 28403833.
- ^ Sims ME (2014-01-01). "Legal Briefs: Iatrogenesis: Prolapsed Umbilical Cord After Artificial Rupture of the Membranes and Unskilled Stabilization". NeoReviews. 15 (1): e32–e36. doi:10.1542/neo.15-1-e32. ISSN 1526-9906.
- ^ "Umbilical Cord Prolapse: Causes, Diagnosis & Management". Cleveland Clinic. Retrieved 2022-04-30.
- ^ Smith JR (2022-04-01). "Postpartum Hemorrhage: Practice Essentials, Problem, Epidemiology". Medscape.
- ^ Demisse GA, Sifer SD, Kedir B, Fekene DB, Bulto GA (March 2019). "Determinants of puerperal sepsis among post partum women at public hospitals in west SHOA zone Oromia regional STATE, Ethiopia (institution BASEDCASE control study)". BMC Pregnancy and Childbirth. 19 (1): 95. doi:10.1186/s12884-019-2230-x. PMC 6423770. PMID 30885159.
- ^ "WHO Technical Consultation on Postpartum Care". World Health Organization. 2010. Retrieved 30 June 2020.
- ^ Jones E, Taylor B, MacArthur C, Pritchett R, Cummins C (February 2016). "The effect of early postnatal discharge from hospital for women and infants: a systematic review protocol". Systematic Reviews. 5: 24. doi:10.1186/s13643-016-0193-9. PMC 4746909. PMID 26857705.
- ^ "Types of Delivery for Pregnancy". Cleveland Clinic. Retrieved 2022-04-30.
- ^ Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H (January 2021). "The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review". Reproductive Health. 18 (1): 10. doi:10.1186/s12978-021-01070-6. PMC 7812564. PMID 33461593.
- ^ a b c Gelis J (1991). History of Childbirth. Boston: Northeastern University Press.
- ^ Healthdirect Australia (2021-05-23). "What do midwives do?". www.pregnancybirthbaby.org.au. Retrieved 2022-04-30.
- ^ a b Adatara P, Amooba PA, Afaya A, Salia SM, Avane MA, Kuug A, et al. (April 2021). "Challenges experienced by midwives working in rural communities in the Upper East Region of Ghana: a qualitative study". BMC Pregnancy and Childbirth. 21 (1): 287. doi:10.1186/s12884-021-03762-0. PMC 8033657. PMID 33836689.
- ^ a b c d Bynum WF, Porter R, eds. (1993). Companion Encyclopedia of the History of Medicine. London and New York: Routledge.
- ^ Carr I (May 2000). "Some Obstetrical History: Dying to Have a Baby - the History of Childbirth" (PDF). University of Manitoba: Women's Health. Retrieved 20 May 2012.
- ^ a b c d e McGrew RE (1985). Encyclopedia of Medical History. New York: McGraw-Hill Book Company.
- ^ a b Hufnagel GL (2012). A History of Women's Menstruation from Ancient Greece to the Twenty-first Century: Psychological, Social, Medical, Religious, and Educational Issues. Lewiston, New York: Edwin Mellen Press.
- ^ International Confederation of Midwives (2022-01-31). "The Origins of Midwifery". ICM. Retrieved 2022-04-30.
- ^ Gasner A, Aatsha PA (2022). "Physiology, Uterus". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32491507. Retrieved 2022-04-30.
- ^ Rhodes P (2004-09-23). "Leake, John (1729–1792), man-midwife". Oxford Dictionary of National Biography. Oxford Dictionary of National Biography (online ed.). Oxford University Press. doi:10.1093/ref:odnb/16239. ISBN 978-0-19-861412-8. (Subscription or UK public library membership required.)
- ^ a b Aziato L, Omenyo CN (March 2018). "Initiation of traditional birth attendants and their traditional and spiritual practices during pregnancy and childbirth in Ghana". BMC Pregnancy and Childbirth. 18 (1): 64. doi:10.1186/s12884-018-1691-7. PMC 5842514. PMID 29514607.
- ^ Al-Gailani S (2018). "Hospital Birth". In Kassell L, Hopwood N, Flemming R (eds.). Reproduction. Cambridge: Cambridge University Press. pp. 553–566. doi:10.1017/9781107705647.046. ISBN 978-1-107-06802-5. S2CID 239583227. Retrieved 2022-04-30.
{{cite book}}:|work=ignored (help) - ^ Sialubanje C, Massar K, Hamer DH, Ruiter RA (September 2015). "Reasons for home delivery and use of traditional birth attendants in rural Zambia: a qualitative study". BMC Pregnancy and Childbirth. 15 (1): 216. doi:10.1186/s12884-015-0652-7. PMC 4567794. PMID 26361976.
- ^ Martell LK (2000). "The hospital and the postpartum experience: a historical analysis". Journal of Obstetric, Gynecologic, and Neonatal Nursing. 29 (1): 65–72. doi:10.1111/j.1552-6909.2000.tb02757.x. PMID 10660278.
- ^ Aborigo RA, Reidpath DD, Oduro AR, Allotey P (January 2018). "Male involvement in maternal health: perspectives of opinion leaders". BMC Pregnancy and Childbirth. 18 (1): 3. doi:10.1186/s12884-017-1641-9. PMC 5749010. PMID 29291711.
- ^ "The Midwives' Registration Bill". The Lancet. Originally published as Volume 2, Issue 3602. 140 (3602): 631–634. 1892-09-10. doi:10.1016/S0140-6736(01)86961-0. ISSN 0140-6736.
- ^ Midwives voices, midwives realities. Findings from a global consultation on providing quality midwifery care (PDF). Switzerland: World Health Organization. 1991. ISBN 978-9241510547.
- ^ a b Drife J (May 2002). "The start of life: a history of obstetrics". Postgraduate Medical Journal. 78 (919): 311–315. doi:10.1136/pmj.78.919.311. PMC 1742346. PMID 12151591..
- ^ Rabinerson D, Horowitz E (May 2007). "[The evolution of midwifery]". Harefuah. 146 (5): 380–4, 405. PMID 17674557.
- ^ Low J (2009). "Caesarean section-past and present" (PDF). Journal of Obstetrics and Gynecology Canada. 31 (12): 1131–1136. doi:10.1016/S1701-2163(16)34373-0. PMID 20085678. Archived from the original (PDF) on January 23, 2013. Retrieved May 20, 2012.
- ^ Caplan CE (1995). "The Childbed Fever Mystery and the Meaning of Medical Journalism". McGill Journal of Medicine. 1 (1). Archived from the original on 2012-07-07.
- ^ Roth J. Pregnancy & Birth: The History of Childbearing Choices in the United States. Human Service Solutions.
- ^ Baskett TF (29 March 2019). "Houstoun, Robert (1678–1734)". Eponyms and Names in Obstetrics and Gynaecology. Cambridge University Press. p. 194. doi:10.1017/9781108421706.154. ISBN 978-1-108-33671-0.
- ^ Lavers A, Yip WS, Sunderland B, Parsons R, Mackenzie S, Seet J, Czarniak P (2018). "Surgical antibiotic prophylaxis use and infection prevalence in non-cosmetic breast surgery procedures at a tertiary hospital in Western Australia-a retrospective study". PeerJ. 6: e5724. doi:10.7717/peerj.5724. PMC 6202972. PMID 30386692.
Table 2: Types of procedures and association with surgical site infections (SSI). P-values were obtained from Fisher's Exact test, unless otherwise specified.
- ^ Vernon LF (August 2019). "J. Marion Sims, MD: Why He and His Accomplishments Need to Continue to be Recognized a Commentary and Historical Review". Journal of the National Medical Association. 111 (4): 436–446. doi:10.1016/j.jnma.2019.02.002. PMID 30851980. S2CID 73725863.
- ^ Rutkow IM (August 1999). "Ephraim McDowell and the world's first successful ovariotomy". Archives of Surgery. 134 (8): 902. doi:10.1001/archsurg.134.8.902. PMID 10443816.
- ^ "Iceman Ötzi may have had tummy trouble when he died". New Scientist. 229 (3056): 17. January 2016. Bibcode:2016NewSc.229...17.. doi:10.1016/s0262-4079(16)30115-4. ISSN 0262-4079.
- ^ Sieber WK (September 1970). "Total prosthetic transplantation of the inferior vena cava, with venous drainage restoration of the one remaining kidney on the graft, successfully performed on a child with Wilms' tumor". Journal of Pediatric Surgery. 5 (6): 694–695. doi:10.1016/s0022-3468(70)80085-9. ISSN 0022-3468.
- ^ a b "Dr. J Marion Sims: The Father of Modern Gynecology". International Wellness Foundation. 12 February 2014.
- ^ Giuliano P (May 2018). "Gender: A Historical Perspective". In Averett SL, Argys LM, Hoffman SD (eds.). The Oxford Handbook of Women and the Economy. Oxford University Press. doi:10.1093/oxfordhb/9780190628963.013.29.
- ^ O'Malley-Keighran MP, Lohan G (December 2016). "Encourages and guides, or diagnoses and monitors: Woman centred-ness in the discourse of professional midwifery bodies". Midwifery. 43: 48–58. doi:10.1016/j.midw.2016.10.007. PMID 27846406.
- ^ "Situation of women and children in Nigeria". www.unicef.org. Retrieved 2022-04-30.
- ^ Bäcklund I (2006). "Modifiers describing women and men in nineteenth-century English". In Kytö M, Rydén M, Smitterberg E (eds.). Nineteenth-Century English. Cambridge: Cambridge University Press. pp. 17–55. doi:10.1017/cbo9780511486944.002. ISBN 9780511486944.
- ^ Adaikan G (January 2020). "Female sexual dysfunction". In Arulkumaran S, Ledger W, Denny L, Doumouchtsis S (eds.). Oxford Textbook of Obstetrics and Gynaecology. Oxford University Press. pp. 743–752. doi:10.1093/med/9780198766360.003.0060. ISBN 978-0-19-876636-0.
- ^ "Uterine Prolapse: Causes, Symptoms, Diagnosis & Treatment". Cleveland Clinic. Retrieved 2022-04-30.



