Pharmacological cardiotoxicity

Pharmacological cardiotoxicity is defined as cardiac damage that occurs under the action of a drug. This can occur both through damage of cardiac muscle as well as through alteration of the ion currents of cardiomyocytes.[1]
Two distinct drug classes in which cardiotoxicity can occur are in anti-cancer and antiarrhythmic drugs. Anti-cancer drug classes that cause cardiotoxicity include anthracyclines, monoclonal antibodies, and antimetabolites. This form generally manifests as a progressive form of heart failure, but can also manifest as an harmful arrhythmia.[2] In contrast, in antiarrhythmic drugs, cardiotoxicity is due to a risk of arrhythmias resulting from treated-induced ion current imbalance.[3]
Other types of drugs are also known for cardiotoxicity, such as clozapine being associated with myocarditis.[4]
Anticancer cardiotoxicity
[edit]The cardiotoxicity of anticancer drugs has been well documented, with an entire sub-speciality of cardio-oncology dedicated towards investigating and treating these serious side effects. Two well known anticancer drug families that cause cardiotoxicity are anthracyclines and monoclonal antibodies targeting HER2. Other types of anticancer drugs that can lead to cardiotoxicity include alkylating agents such as cyclophosphamide, BCR-ABL1 targeting receptor tyrosine kinases such as imatinib, and VEGF antibodies such as bevicizumab.[5] This section of the article will focus on anthracyclines and HER2 monoclonal antibodies due to the prominence of cardiotoxicity in these compounds.
Pathophysiology
[edit]The mechanism of anthracycline-induced cardiotoxicity is unknown and is under active research. However, multiple theories exist. One well supported mechanism is related to the production of superoxide anion radicals that in turn damage cardiac myocytes. [6] Recent research suggests that Top2b (topoisomerase-IIβ) helps mediate the production of oxygen radicals, representing a potential biomarker for this serious side effect.[7] Other proposed mechanisms include interference with cardiac ATP production, mitochondria-related stress, and lipid peroxidation.[6]
On the other hand, the mechanism of HER2 antibody cardiotoxicity is more well known. [8] HER2 is a protein expressed on the cell membranes of HER2 positive breast cancer cells. However, HER2 is also expressed on the surface of cardiac myocytes. It is hypothesized that HER2 expressed in these cardiac cells have a cardioprotective mechanism, and the targeting of these proteins in this context leads to the cardiotoxicity associated with HER2 monoclonal antibodies.[9]
Clinical Manifestation and Epidemiology
[edit]The cardiotoxicity of anthracyclines can be classified into three categories: early, early onset chronic, and late onset chronic. Early cardiotoxicity is rare, but manifests as arrthymias, myocarditis, and pericarditis. This type of toxicity occurs directly after treatment with anthracycline. Early onset chronic cardiotoxicity is defined as cardiotoxicity manifesting within one year of the completion of treatment, while late onset chronic cardiotoxicity occurs after one year. [10] The cardiotoxicity of anthracyclines is dose dependent. At total exposure levels lower than 400 mg/m2, the incidence of heart failure is between 3%-5%. At a exposure rate of 700 mg/m2, the heart failure rate is at 48%.[11]
Cardiotoxicity involving HER2 monoclonal antibodies manifests as decrease left ventricular ejection fraction and resulting heart failure.[12] The cardiotoxicity of HER2 monoclonal antibodies is dose independent.[13]
Treatments
[edit]The immediate intervention for the development of cardiotoxicity is discontinuation of the drug. Preventative measures for anthracycline induced cardiomyopathy include dexrazoxane, which is the only preventative drug approved by the FDA for prevention of anthracycline cardiomyopathy.[14] Overall, there are no specific treatments targeted towards the cardiotoxicity of anticancer drugs. Rather, treatment is of the resultant heart failure. This often takes the form of ACE inhibitors or beta blockers. [15]
Antiarrhymic cardiotoxicity
[edit]
Antiarrhythmics are broad class of drugs that are used treat heart rhythm irregularities. [16] Utilizing the Vaughan-Williams (VW) system, antiarrhymic drugs are classified into four main classes based on their mechanism of action. Class I antiarrhymics lead to blockage of sodium channels. Class II antiarrhymatics are beta-adrenoceptor blockers. Class III antiarrhymics act as potassium channel blockers, while Class IV antiarrhymics are non-dihydropyridine calcium channel blockers. While the effects of these drugs may be antiarrhymic, they can also be proarrhymic in other contexts.
Pathophysiology
[edit]The pharmacological cardiotoxicity of antiarrhymic compounds is related to their electrophysiological mechanism. In particular, because antiarrhymics drugs act on the opening/closing of ion channels, the modification of the electrical currents can lead to adverse cardiac events such torsade de pointes or ventricular fibrillation. Due to the case-by-case basis in which these medication lead to cardiotoxicity and the development of specific adverse rhythms, it has become increasingly important to assess compounds in a preclinical environment (See Pharmacological cardiotoxicity#In Silico Cardiotoxicity Assessment).
Clinical Manifestation and Epidemiology
[edit]The manifestation of antiarrhymic cardiotoxicity may manifest as worsening of the pre-existent arrhythmia or the development of a new arrhythmia.
Female sex at birth has been associated with an increased risk of the development of new arrhythmia, and other risk factors include age, kidney disease, drug-drug interactions, and other underlying heart problems.[17]
Treatment
[edit]Like with anticancer drugs, the most common intervention for the development of cardiotoxicity is discontinuation of the causative drug. Individual risk factors, such as risk of arrhythmia re-emergence, are considered when deciding final courses of action. Adjacent devices, such as pacemakers, or ablation therapy may also be considered as alternatives to medical treatment for the primary arrhythmia.[18]
The treatment of torsade de pointes is typically with intravenous magnesium sulfate, which helps stabilize cardiac membranes.[19] For ventricular fibrillation cases, either/or defibrillation, amiodarone, or epinephrine is used dependent on the ACLS algorithm. [20]
In silico cardiotoxicity assessment
[edit]Background
[edit]In the last years, in silico models have aided scientists and clinicians to cure several diseases.[21] Computational modeling in particular has helped scientists to alter parameters that otherwise could have not been investigated.[21]
In the field of electrophysiology, pharmacological cardiotoxicity can be carried out by leveraging specific computational models. Recently, it has become possible to analyze the pharmacological effect on atria and ventricles separately.[22][23]
Since the two cardiac chambers are very different each other and play a key role both on a functional and anatomical basis, suitable computational models have to be accounted for to describe their different behavior. During the years, several models have been developed to best characterize and replicate the cellular action potential behavior of the most relevant anatomical region of the heart, such as Courtemanche model for atria or O'Hara model for ventricles.[22][23]
Creation of a population of cellular action potentials
[edit]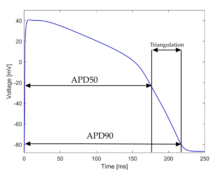
In this way, it has been possible to create a virtual cellular population of cardiomyocytes and vary their conductances that are related to the main ionic currents which contribute to the action potential morphology, and is reflective of a specific anatomical region of the heart.[24][25]
In order to create a stable population of cellular action potentials, several biomarkers have been developed to best characterize the instability of cellular action potentials. Examples of biomarkers reported include:[24]
- APD90: it represents the action potential duration when the phase of the repolarization is at 90%, so it is possible to associate to this value a time and it can be expressed as:[26]
- APD90: it represents the action potential duration when the phase of the repolarization is at 50%, so it is possible to associate to this value a time and it can be expressed as:[26]
- APD20: it represents the action potential duration when the phase of the repolarization is at 20%, so it is possible to associate to this value a time and it can be expressed as:[26]
- Triangulation: it is a measure of how triangular is an action potential, expressed as:[26]
- APA: it represents the action potential amplitude, expressed as:[26]
Regional clusterization
[edit]Once the cellular population is stable, all action potential are then compared to physiological data related to the most relevant anatomical regions to appropriately filter the action potential, aiming to consider just the physiologically relevant ones.[27]
At the atrial level, clusterization occurs with data associated to:[27]
- Right atrium
- Right atrial appendage
- Left atrium
- Left atrial appendage
- Atrioventricular rings
- Crista terminalis
- Right Bachmann's bundle
- Left Bachmann's bundle
- Pectinate muscles
Simulation of the pharmacological action
[edit]
According to pharmacokinetic and pharmacodynamic ideals, pharmacological action is integrated in the model. By means of specific electrical stimuli protocols,[28] the pharmacological effect of a new drug can be investigated in a completely safe, and controlled computational environment, providing preliminary important considerations concerning the cardiotoxicity of new pharmacological compounds.[29]
According to the outcome of the simulations, several aspects can be investigated to identify the proarrhythmicity of a new pharmacological compound.[30][31] The typical changes, known as repolarization abnormalities, that are considered pro-arrhythmic include:[31]
- Early afterdepolarization
- Electrical alternans
- Repolarization failures
Torsade de point risk score
[edit]Simulation can be carried out at different effective plasmatic therapeutic level of the drugs to identify the level at which cardiotoxicity cannot be neglected. The data collected could be finally managed to create a score system aimed to define the torsadogenic risk, namely the risk of inducing torsade de pointes, of the new drugs.[32][33]
A possible torsade de point risk score to assess cardiotoxicity could be:[33]
where is the sum of all concentrations, [C] is the concentration taken into account, , is the total number of models in the population, and represents the number of models showing repolarization abnormalities.[33]
Tissue simulations
[edit]More detailed computation simulations can be carried out accounting for not cellular models, but taking into consideration the functional syncytium and enabling the cells to mutually interact, the so-called electrotonic coupling.[34]
In case of tissue simulation or in wider cases, such as in whole organ simulations, all the cellular models are note applicable anymore, and several corrections have to be made. Firstly, the governing equations can not be just ordinary differential equations, but a system of partial differential equations has to be accounted for.[35] A suitable choice may be the monodomain model:[36]
where is the effective conductivity tensor, is the capacitance of the cellular membrane, the transmembrane ionic current, and are the domain of interest and its boundary, respectively, with the outward boundary of .[36]
See also
[edit]References
[edit]- ^ Iqubal, A.; Ehtaishamul Haque, S.; Sharma, S.; Asif Ansari, M. (2018). "Clinical Updates on Drug-Induced Cardiotoxicity". International Journal of Pharmaceutical Sciences and Research. 9 (1): 16–26. doi:10.13040/IJPSR.0975-8232.9(1).16-26.
- ^ Ewer, Michael S.; Ewer, Steven M. (September 2015). "Cardiotoxicity of anticancer treatments". Nature Reviews Cardiology. 12 (9): 547–558. doi:10.1038/nrcardio.2015.65. ISSN 1759-5002. PMID 25962976. S2CID 9317756.
- ^ Ramalingam, Mahesh; Kim*, Sung-Jin (2016). "Pharmacological Activities and Applications of Spicatoside A". Biomolecules & Therapeutics (Biomolecules & Therapeutics). 24 (5): 469–474. doi:10.4062/biomolther.2015.214. PMC 5012870. PMID 27169821.
- ^ Patel, Rishi K.; Moore, Alice M.; Piper, Susan; Sweeney, Mark; Whiskey, Eromona; Cole, Graham; Shergill, Sukhi S.; Plymen, Carla M. (2019-12-01). "Clozapine and cardiotoxicity – A guide for psychiatrists written by cardiologists". Psychiatry Research. 282: 112491. doi:10.1016/j.psychres.2019.112491. ISSN 0165-1781. PMID 31351758.
- ^ Gao, Feiyu; Xu, Tao; Zang, Fangnan; Luo, Yuanyuan; Pan, Defeng (2024-09-12). "Cardiotoxicity of Anticancer Drugs: Molecular Mechanisms, Clinical Management and Innovative Treatment". Drug Design, Development and Therapy. 18: 4089–4116. doi:10.2147/DDDT.S469331. PMC 11404500. PMID 39286288.
- ^ a b Raj, Shashi; Franco, Vivian I.; Lipshultz, Steven E. (2014-04-22). "Anthracycline-Induced Cardiotoxicity: A Review of Pathophysiology, Diagnosis, and Treatment". Current Treatment Options in Cardiovascular Medicine. 16 (6): 315. doi:10.1007/s11936-014-0315-4. ISSN 1534-3189. PMID 24748018.
- ^ Zhang, Sui; Liu, Xiaobing; Bawa-Khalfe, Tasneem; Lu, Long-Sheng; Lyu, Yi Lisa; Liu, Leroy F.; Yeh, Edward T. H. (November 2012). "Identification of the molecular basis of doxorubicin-induced cardiotoxicity". Nature Medicine. 18 (11): 1639–1642. doi:10.1038/nm.2919. ISSN 1546-170X. PMID 23104132.
- ^ Keefe, Deborah L. (October 2002). "Trastuzumab-associated cardiotoxicity". Cancer. 95 (7): 1592–1600. doi:10.1002/cncr.10854. ISSN 0008-543X. PMID 12237930.
- ^ Copeland-Halperin, Robert S.; Liu, Jennifer E.; Yu, Anthony F. (July 2019). "Cardiotoxicity of HER2-targeted therapies". Current Opinion in Cardiology. 34 (4): 451–458. doi:10.1097/HCO.0000000000000637. ISSN 0268-4705. PMC 7313632. PMID 31082851.
- ^ Volkova, Maria; Russell, Raymond (2012). "Anthracycline Cardiotoxicity: Prevalence, Pathogenesis and Treatment". Current Cardiology Reviews. 7 (4): 214–220. doi:10.2174/157340311799960645. PMC 3322439. PMID 22758622.
- ^ Johnson, Mark; Keyes, Daniel (2024), "Anthracycline Toxicity", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 38261713, retrieved 2024-11-12
- ^ "Cardiotoxicity and the Evolving Landscape of HER2-Targeted Breast Cancer Treatment". American College of Cardiology. Retrieved 2024-11-12.
- ^ Zhang, Li; Wang, Yan; Meng, Wenjing; Zhao, Weipeng; Tong, Zhongsheng (2022-08-22). "Cardiac safety analysis of anti-HER2-targeted therapy in early breast cancer". Scientific Reports. 12 (1): 14312. Bibcode:2022NatSR..1214312Z. doi:10.1038/s41598-022-18342-1. ISSN 2045-2322. PMC 9395410. PMID 35995984.
- ^ de Baat, Esmée C; Mulder, Renée L; Armenian, Saro; Feijen, Elizabeth AM; Grotenhuis, Heynric; Hudson, Melissa M; Mavinkurve-Groothuis, Annelies MC; Kremer, Leontien CM; van Dalen, Elvira C (2022-10-27). "Dexrazoxane for preventing or reducing cardiotoxicity in adults and children with cancer receiving anthracyclines". Cochrane Database Systematic Reviews. 9 (9): CD014638. doi:10.1002/14651858.CD014638.pub2. PMC 9512638. PMID 36162822.
- ^ Shakir, Douraid (2009). "Chemotherapy Induced Cardiomyopathy: Pathogenesis, Monitoring and Management". Journal of Clinical Medicine Research. 1 (1): 8–12. doi:10.4021/jocmr2009.02.1225. ISSN 1918-3003. PMC 3318862. PMID 22505958.
- ^ King, Gregory S.; Goyal, Amandeep; Grigorova, Yulia; Patel, Preeti; Hashmi, Muhammad F. (2024), "Antiarrhythmic Medications", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29493947, retrieved 2024-11-15
- ^ Dan, Gheorghe-Andrei; Martinez-Rubio, Antoni; Agewall, Stefan; Boriani, Giuseppe; Borggrefe, Martin; Gaita, Fiorenzo; van Gelder, Isabelle; Gorenek, Bulent; Kaski, Juan Carlos; Kjeldsen, Keld; Lip, Gregory Y. H.; Merkely, Bela; Okumura, Ken; Piccini, Jonathan P.; Potpara, Tatjana (2018-05-01). "Antiarrhythmic drugs-clinical use and clinical decision making: a consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology (ESC) Working Group on Cardiovascular Pharmacology, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and International Society of Cardiovascular Pharmacotherapy (ISCP)". Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology. 20 (5): 731–732an. doi:10.1093/europace/eux373. ISSN 1532-2092. PMID 29438514.
- ^ Dan, Gheorghe-Andrei; Martinez-Rubio, Antoni; Agewall, Stefan; Boriani, Giuseppe; Borggrefe, Martin; Gaita, Fiorenzo; van Gelder, Isabelle; Gorenek, Bulent; Kaski, Juan Carlos; Kjeldsen, Keld; Lip, Gregory Y. H.; Merkely, Bela; Okumura, Ken; Piccini, Jonathan P.; Potpara, Tatjana (2018-05-01). "Antiarrhythmic drugs-clinical use and clinical decision making: a consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology (ESC) Working Group on Cardiovascular Pharmacology, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and International Society of Cardiovascular Pharmacotherapy (ISCP)". Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology. 20 (5): 731–732an. doi:10.1093/europace/eux373. ISSN 1532-2092. PMID 29438514.
- ^ Cohagan, Brian; Brandis, Dov (2024), "Torsade de Pointes", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29083738, retrieved 2024-11-20
- ^ "VTach ACLS Training | Advanced Cardiac Life Support". ACLS Medical Training. Retrieved 2024-11-20.
- ^ a b Viceconti, Marco; Dall'Ara, Enrico (January 2019). "From bed to bench: How in silico medicine can help ageing research". Mechanisms of Ageing and Development. 177: 103–108. doi:10.1016/j.mad.2018.07.001. hdl:11585/658491. PMID 30005915. S2CID 49661463.
- ^ a b Courtemanche, Marc; Ramirez, Rafael J.; Nattel, Stanley (1998-07-01). "Ionic mechanisms underlying human atrial action potential properties: insights from a mathematical model". American Journal of Physiology. Heart and Circulatory Physiology. 275 (1): H301–H321. doi:10.1152/ajpheart.1998.275.1.H301. ISSN 0363-6135. PMID 9688927.
- ^ a b O'Hara, Thomas; Virág, László; Varró, András; Rudy, Yoram (2011-05-26). McCulloch, Andrew D. (ed.). "Simulation of the Undiseased Human Cardiac Ventricular Action Potential: Model Formulation and Experimental Validation". PLOS Computational Biology. 7 (5): e1002061. Bibcode:2011PLSCB...7E2061O. doi:10.1371/journal.pcbi.1002061. ISSN 1553-7358. PMC 3102752. PMID 21637795.
- ^ a b Muszkiewicz, Anna; Britton, Oliver J.; Gemmell, Philip; Passini, Elisa; Sánchez, Carlos; Zhou, Xin; Carusi, Annamaria; Quinn, T. Alexander; Burrage, Kevin; Bueno-Orovio, Alfonso; Rodriguez, Blanca (January 2016). "Variability in cardiac electrophysiology: Using experimentally-calibrated populations of models to move beyond the single virtual physiological human paradigm". Progress in Biophysics and Molecular Biology. 120 (1–3): 115–127. doi:10.1016/j.pbiomolbio.2015.12.002. PMC 4821179. PMID 26701222. S2CID 13737964.
- ^ Sarkar, Amrita X.; Christini, David J.; Sobie, Eric A. (2012-06-01). "Exploiting mathematical models to illuminate electrophysiological variability between individuals: Electrophysiological variability". The Journal of Physiology. 590 (11): 2555–2567. doi:10.1113/jphysiol.2011.223313. PMC 3424714. PMID 22495591.
- ^ a b c d e Lachaud, Quentin; Aziz, Muhamad Hifzhudin Noor; Burton, Francis L; Macquaide, Niall; Myles, Rachel C; Simitev, Radostin D; Smith, Godfrey L (2022-12-09). "Electrophysiological heterogeneity in large populations of rabbit ventricular cardiomyocytes". Cardiovascular Research. 118 (15): 3112–3125. doi:10.1093/cvr/cvab375. ISSN 0008-6363. PMC 9732512. PMID 35020837.
- ^ a b Ferrer, Ana; Sebastián, Rafael; Sánchez-Quintana, Damián; Rodríguez, José F.; Godoy, Eduardo J.; Martínez, Laura; Saiz, Javier (2015-11-02). Panfilov, Alexander V (ed.). "Detailed Anatomical and Electrophysiological Models of Human Atria and Torso for the Simulation of Atrial Activation". PLOS ONE. 10 (11): e0141573. Bibcode:2015PLoSO..1041573F. doi:10.1371/journal.pone.0141573. ISSN 1932-6203. PMC 4629897. PMID 26523732.
- ^ Abi-Gerges, Najah; Small, Ben G; Lawrence, Chris L; Hammond, Tim G; Valentin, Jean-Pierre; Pollard, Chris E (March 2006). "Gender differences in the slow delayed ( I Ks ) but not in inward ( I K1 ) rectifier K + currents of canine Purkinje fibre cardiac action potential: key roles for I Ks , β -adrenoceptor stimulation, pacing rate and gender: Gender, pacing rate and stimulated I Ks". British Journal of Pharmacology. 147 (6): 653–660. doi:10.1038/sj.bjp.0706491. PMC 1751338. PMID 16314855.
- ^ Passini, Elisa; Britton, Oliver J.; Lu, Hua Rong; Rohrbacher, Jutta; Hermans, An N.; Gallacher, David J.; Greig, Robert J. H.; Bueno-Orovio, Alfonso; Rodriguez, Blanca (2017). "Human In Silico Drug Trials Demonstrate Higher Accuracy than Animal Models in Predicting Clinical Pro-Arrhythmic Cardiotoxicity". Frontiers in Physiology. 8: 668. doi:10.3389/fphys.2017.00668. ISSN 1664-042X. PMC 5601077. PMID 28955244.
- ^ Smith, J M; Clancy, E A; Valeri, C R; Ruskin, J N; Cohen, R J (January 1988). "Electrical alternans and cardiac electrical instability". Circulation. 77 (1): 110–121. doi:10.1161/01.CIR.77.1.110. ISSN 0009-7322. PMID 3335062.
- ^ a b Weiss, James N.; Garfinkel, Alan; Karagueuzian, Hrayr S.; Chen, Peng-Sheng; Qu, Zhilin (December 2010). "Early afterdepolarizations and cardiac arrhythmias". Heart Rhythm. 7 (12): 1891–1899. doi:10.1016/j.hrthm.2010.09.017. ISSN 1547-5271. PMC 3005298. PMID 20868774.
- ^ Tisdale, James E.; Jaynes, Heather A.; Kingery, Joanna R.; Mourad, Noha A.; Trujillo, Tate N.; Overholser, Brian R.; Kovacs, Richard J. (July 2013). "Development and Validation of a Risk Score to Predict QT Interval Prolongation in Hospitalized Patients". Circulation: Cardiovascular Quality and Outcomes. 6 (4): 479–487. doi:10.1161/CIRCOUTCOMES.113.000152. ISSN 1941-7713. PMC 3788679. PMID 23716032.
- ^ a b c Fogli Iseppe, Alex; Ni, Haibo; Zhu, Sicheng; Zhang, Xianwei; Coppini, Raffaele; Yang, Pei-Chi; Srivatsa, Uma; Clancy, Colleen E.; Edwards, Andrew G.; Morotti, Stefano; Grandi, Eleonora (August 2021). "Sex-Specific Classification of Drug-Induced Torsade de Pointes Susceptibility Using Cardiac Simulations and Machine Learning". Clinical Pharmacology & Therapeutics. 110 (2): 380–391. doi:10.1002/cpt.2240. ISSN 0009-9236. PMC 8316283. PMID 33772748.
- ^ del Rio, Carlos; Hamlin, Robert; Billman, George (2016-09-01). "Myocardial electrotonic coupling modulates repolarization heterogeneities in vivo: Implications for the assessment of pro-arrhythmic liabilities in vitro and in silico". Journal of Pharmacological and Toxicological Methods. Focused Issue on Safety Pharmacology. 81: 354. doi:10.1016/j.vascn.2016.02.063. ISSN 1056-8719. S2CID 89280007.
- ^ Sundnes, Joakim; Nielsen, Bjørn Fredrik; Mardal, Kent Andre; Cai, Xing; Lines, Glenn Terje; Tveito, Aslak (2006-07-01). "On the Computational Complexity of the Bidomain and the Monodomain Models of Electrophysiology". Annals of Biomedical Engineering. 34 (7): 1088–1097. doi:10.1007/s10439-006-9082-z. ISSN 1573-9686. PMID 16773461. S2CID 17230936.
- ^ a b Mountris, Konstantinos A.; Dong, Leiting; Guan, Yue; Atluri, Satya N.; Pueyo, Esther (2022-11-01). "A meshless fragile points method for the solution of the monodomain model for cardiac electrophysiology simulation". Journal of Computational Science. 65: 101880. doi:10.1016/j.jocs.2022.101880. ISSN 1877-7503. S2CID 252975713.








![{\displaystyle W_{c}={\frac {EFTPC}{[C]}}}](https://wikimedia.org/api/rest_v1/media/math/render/svg/7de6649384bef4c5b47eb55f2be0f7de6b2ed1ad)










