OXGR1
| OXGR1 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | OXGR1, GPR80, GPR99, P2RY15, P2Y15, aKGR, oxoglutarate receptor 1 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 606922; MGI: 2685145; HomoloGene: 25878; GeneCards: OXGR1; OMA:OXGR1 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
OXGR1, i.e., 2-oxoglutarate receptor 1 (also known as GPR99, cysteinyl leukotriene receptor E, i.e., CysLTE, and cysteinyl leukotriene receptor 3, i.e., CysLT3[5][6]) is a G protein-coupled receptor located on the surface membranes of certain cells. It functions by binding one of its ligands and thereby becoming active in triggering pre-programmed responses in its parent cells. OXGR1 has been shown to be activated by α-ketoglutarate,[7] itaconate,[8] and three cysteinyl-containing leukotrienes (abbreviated as CysLTs), leukotriene E4 (i.e., LTE4), LTC4, and LTD4.[5][9] α-Ketoglutarate and itaconate are the dianionic forms of α-ketoglutaric acid and itaconic acid, respectively. α-Ketoglutaric and itaconic acids are short-chain dicarboxylic acids that have two carboxyl groups (notated as -CO2H) both of which are bound to hydrogen (i.e., H+). However, at the basic pH levels (i.e., pH>7) in virtually all animal tissues, α-ketoglutaric acid and itaconic acid exit almost exclusively as α-ketoglutarate and itaconate, i.e., with their carboxy residues being negatively charged (notated as -CO2), because they are not bound to H+ (see Conjugate acid-base theory). It is α-ketoglutarate and itaconate, not α-ketoglutaric or itaconic acids, which activate OXGR1.[7][8]
History
[edit]In 2001, a human gene projected to code for a G protein-coupled receptor (i.e., a receptor that stimulates cells by activating G proteins) was identified. Its protein product was classified as an orphan receptor, i.e., a receptor whose activating ligand and function are unknown. The projected amino acid sequence of the protein encoded by this gene bore similarities to the purinergic receptor, P2Y1, and therefore might, like P2Y1, be a receptor for purines. This study named the new receptor and its gene GPR80 and GPR80, respectively.[10] Shortly thereafter, a second study found this same gene, indicated that it coded for a G protein-coupled receptor, had an amino acid sequence similar to two purinergic receptors, P2Y1 and GPR91, and determined that a large series of purine nucleotides, other nucleotides, and derivatives of these compounds did not activate this receptor. The study named this receptor GPR99.[11] A third study published in 2004 reported an orphan G protein-coupled receptor with an amino acid sequence similar to the P2Y receptor family of nucleotides was activated by two purines, adenosine and adenosine monophosphate. The study nominated this receptor to be a purinergic receptor and named it the P2Y15 receptor.[12] However, a review in 2004 of these three studies by members of the International Union of Pharmacology Subcommittee for P2Y Receptor Nomenclature and Classification decided that GPR80/GPR99 is not a receptor for adenosine, adenosine monophosphate, or any other nucleotide.[13] A fourth study, also published in 2004, found that GPR80/GPR99 -bearing cells responded to α-ketoglutarate.[14] In 2013, IUPHAR accepted this report and the names OXGR1 and OXGR1 for the α-ketoglutarate responsive receptor and its gene, respectively.[15] In 2013, a fifth study found that LTE4, LTC4, and LTD4 activated OXGR1.[5] Finally, a 2023 study provided evidence that itaconate also activated OXGR1.[8][16]
OXGR1 gene
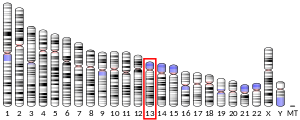
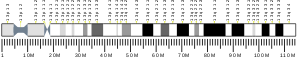
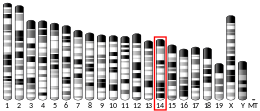
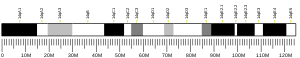
[edit]The human OXGR1 gene is located on chromosome 13 at position 13q32.2; that is, it resides at position 32.2 (i.e., region 3, band 2, sub-band 2) on the "q" arm (i.e., long arm) of chromosome 13.[11][17] OXGR1 codes for a G protein coupled-receptor that is primarily linked to and activates heterotrimeric G proteins containing the Gq alpha subunit. When bound to one of its ligands, OXGR1 activates Gq alpha subunit-regulated cellular pathways (see Functions of the Gq alpha pathways) that stimulate the cellular responses that these pathways are programmed to elicit.[18][19]
OXGR1 activating and inhibiting ligands
[edit]Activating ligands
[edit]OXGR1 is the receptor for α-ketoglutarate, LTE4, LTC4, LTD4, and itaconate. These ligands have the following relative potencies in stimulating responses in cultures of cells expressing human OXGR1:[8]
- LTE4 >> LTC4 = LTD4 > α-ketoglutarate = itaconate
LTE4 is able to stimulate responses in at least some of its target cells at concentrations as low as a few picomoles/liter[5][8] whereas LTC4, LTD4, α-ketoglutarate, and itaconate require far higher levels to do so.[6][16]
The relative potencies that LTC4, LTD4, and LTE4 have in activating their target receptors, i.e., cysteinyl leukotriene receptor 1 (CysLTR1), cysteinyl leukotriene receptor 2 (CysLTR2), and OXGR1 are:[6]
- CysLTR1: LTD4 > LTC4 >> LTE4
- CysLTR2: LTC4 = LTD4 >> LTE4
- OXGR1: LTE4 > LTC4 > LTD4
These relationships suggest that CysTR1 and CysLTR2 are physiological receptors for LTD4 and LTC4 but due to its relative weakness in stimulating these two receptors, perhaps not or to a far lesser extent for LTE4. Indeed, the LTE4 concentrations needed to activate CysTR1 and CysLTR2 may be higher than those that normally occur in vivo (see Functions of OXGR1 in mediating the actions of LTE4, LTD4, and LTC4). These potency relationships suggest that the LTE4's actions are mediated primarily by OXGR1. The following findings support this suggestion. First, pretreatment of guinea pig trachea and human bronchial smooth muscle with LTE4 but not with LTC4 or LTD4 enhanced their smooth muscle contraction responses to histamine. This suggests LTE4's target receptor differs from the receptors targeted by LTC4 and LTD4. Second, LTE4 was as potent as LTC4 and LTD4 in eliciting vascular leakage when injected into the skin of guinea pigs and humans; the inhalation of LTE4 by asthmatic individuals caused the accumulation of eosinophils and basophils in their bronchial mucosa whereas the inhalation of LTD4 did not have this effect; and mice engineered to lack CysLTR1 and CysLTR2 receptors exhibited edema responses to the intradermal injection of LTC4, LTD4, and LTE4 but LTE4 was 64-fold more potent in triggering this response in these mice than in wild type mice. Since LTE4 should have been far less active than LTC4 or LTD4 in triggering vascular leakage, the recruitment of the cited cells into the lung, and causing vascular edema responses in mice lacking CysLT1 and CysLT2 receptors, these findings imply that the latter two receptors are not the primary receptors mediating LTF4' actions. And third, mice engineered to lack all three CysLTR1, CysLTR2, and OXGR1 receptors did not exhibit dermal edema responses to the injection of LTC4, LTD4, or LTE4 thereby indicating that at least one of these receptors was responsible for each of their actions. Overall, these findings suggest that LTE4 commonly acts through a different receptor than LTC4 and LTD4 and that this receptor is OXGR1.[5][9][20] Indeed, studies have defined OXGR1 as the high affinity receptor for LTF4.[9][21] Nonetheless, several studies have reported that cultures of certain types of inflammatory cells, e.g., the human LAD2 (but not LUVA) mast cell lines,[22] T helper cell lymphocytes that have differentiated into Th2 cells,[23] and mouse ILC2 lymphocytes (also termed type 2 innate lymphoid cells)[24] The levels of LTE4 used in some of these studies may not develop in animals or humans. In all events, dysfunctions caused by deleting the OXGR1 gene in cells, tissues or animals and dysfunctions in humans that are associated with a lack of a viable OXGR1 gene implicate the lack of OXGR1 protein in the development of these dysfunctions.[9][22]
Inhibiting ligand
[edit]OXGR1 is inhibited by Montelukast, a well-known and clinically useful receptor antagonist, i.e., inhibitor, of CysLTR1 but not CysTR2 activation. (Inhibitors of CysLTR2 have not been identified.[25]) In consequence, Montelukast blocks the binding and thereby the actions of LTE4, LTC4, and LTD4 that are mediated by OXGR1. It is presumed to act similarly to block the actions of α-ketoglutarate and itaconate on OXGR1.[5][26] It is not yet known if other CysLTR1 inhibitors can mimic Montelukast in blocking OXGR1's responses to α-ketoglutarate and itaconate. Montelukast is used to treat various disorders including asthma, exercise-induced bronchoconstriction, allergic rhinitis, primary dysmenorrhea (i.e. menstrual cramps not associated with known causes, see causes of dysmenorrhea), and urticaria (see Functions of CysLTR1). While it is likely that its inhibition of CysLTR1 accounts for its effects in these diseases, the ability of these leukotrienes, particularly LTE4, to stimulate OXGR1 allows that Montelukast's effects on these conditions may be due at least in part to its ability to block OXGR1.[5]
Expression
[edit]Based on their content of the OXGR1 protein or mRNA that directs its synthesis, OXGR1 is expressed in human: a) kidney, placenta, and fetal brain; b) cells that promote allergic and other hypersensitivity reactions, i.e., eosinophils and mast cells; c) tissues involved in allergic and other hypersensitivity reactions such as the lung trachea, salivary glands, and nasal mucosa;[5][27][28] and d) fibroblasts, i.e., cells that synthesize the extracellular matrix and collagen (when pathologically activated, these cells produce tissue fibrosis).[25] In mice, Oxgr1 mRNA is highly expressed in kidneys, testes, smooth muscle tissues,[5] nasal epithelial cells, and lung epithelial cells.[29]
Functions
[edit]Associated with OXGR1 gene defects or deficiencies
[edit]The following studies have defined OXGR1 functions based on the presence of disorders in mice or humans that do not have a viable OXGR1 protein. It is not been determined which of OXGR1's ligands, if any, are responsible for stimulating OXGR1 to prevent these disorders.
Otitis media
[edit]Mice lacking OXGPR1 protein due the knockout of their OXGR1 gene developed (82% penetrance) otitis media (i.e., inflammation in their middle ears), mucus effusions in their middle ears, and hearing losses all which had many characteristics of human otitis media. The study did not find evidence that these mice had a middle ear bacterial infection. (Infection with Streptococcus pneumoniae, Moraxella catarrhalis, or other bacteria is one of the most common causes of otitis media.[30]) While the underlying mechanism for the development of this otitis has not been well-defined, the study suggests that OXER1 functions to prevent middle ear inflammations and Oxgr1 gene knockout mice may be a good model to study and relate to human ear pathophysiology.[31]
Goblet cells
[edit]Mice lacking OXGR1 protein due the knockout of their OXGR1 gene had significantly fewer numbers of mucin-containing goblet cells in their nasal mucosa than control mice. Cysltr1 gene knockout mice and Cysltr2 gene knockout mice had normal numbers of these nasal goblet cells. This finding implicates OXGR1 in functioning to maintain higher numbers of airway goblet cells.[29]
Kidney stones and nephrocalcinosis
[edit]Majmunda et al. identified 6 individuals from different families with members that had histories of developing calcium-containing kidney stones (also termed nephrolithiasis) and/or nephrocalcinosis (i.e., the deposition of calcium-containing material in multiple sites throughout the kidney). Each of these 6 individuals had dominant variants in their OXGR1 gene. These variant genes appeared (based on their OXGR1 gene's DNA structure as defined by exome sequencing) to be unable to form an active OXGR1 protein. The study proposed that the OXGR1 gene is a candidate for functioning to suppress the development of calcium-containing nephrolithiasis and nephrocalcinosis in humans.[32]
Associated with α-ketoglutarate-regulated functions
[edit]Studies in rodents have found that the ability of α-ketoglutarate to regulate various functions is dependent on its activation of OXGR1 (see OXGR1 receptor-dependent bioactions of α-ketoglutarate). These functions include: promoting normal kidney functions such as the absorption of key urinary ions and maintenance of acid base balance;[33] regulating the development of glucose tolerance as defined by glucose tolerance tests;[34] suppressing the development of diet-induced obesity;[35] and suppressing the muscle atrophy response to excessive exercise.[35]
Associated with LTE4-induced functions
[edit]A study showed that LTE4, LTC4, and LTD4 produce similar levels of vascular leakage and localized tissue swelling when injected into the skin of guinea pigs or humans. Studies that examined the effects of using various doses of these LTs after injection into the earlobes of mice found that, in comparison to control mice, OXGR1 gene knockout mice showed virtually no response to injection of a low dose of LTE4, a greatly reduced response to injection of an intermediate dose of LTE4, and a somewhat delayed but otherwise similar response to a high dose of LTE4 (these doses were 0.008, 0.0625, and 0.5 nmols, respectively). The study concluded that lower levels of LTE4 act primarily through OXGR1 to cause vascular permeability and, since it is the major cysteinyl leukotriene that accumulates in inflamed tissues, suggested that OXGR1 may be a therapeutic target for treating inflammatory disorders.[5] Another study found that the application of an extract of Alternaria alternata (a genus of fungi that infects plants and causes allergic diseases, infections, and toxic reactions in animals and humans[36]) into the noses of mice caused their nasal epithelial cells to release mucin and their nasal submucosa to swell. (The nasal as well as lung epithelial cells of these mice expressed OXGR1). OXGR1 gene knockout mice did not show these responses to the fungal toxin. The study also showed that a) Cysltr1 and Cysltr2 double gene knockout mice had full mucin release response to the toxin and b) Cstlr2 gene knockout mice had full submucosal swelling responses to the toxin but Csltr1 gene knockout mice did not show submucosal swelling responses to the toxin. The study concluded that LTE4's activation of OXGR1 controls key airway epithelial cell functions in mice and suggested that the inhibition of LTE4-induced OXGR1 activation may prove useful for treating asthma and other allergic and inflammatory disorders.[29] A subsequent study examined the effects of LTE4-OXGR1 on a certain type of tuft cell. When located in intestinal mucosa, these tuft cells are termed tuft cells but when located in the nasal respiratory mucosa they are termed solitary chemosensory cells and when located in the trachea they are termed brush cells.[37] Control mice that inhaled the mold Alternaria alternata, the American house dust mite Dermatophagoides farinae, or LTF4 developed increases in the number of their tracheal brush cells, release of the inflammation-promoting cytokine, interleukin 25, and lung inflammation whereas OXGR1 gene knockout mice did not show these responses. These findings indicate that the activation of OXGR1 regulates airway: brush cell numbers, interleukin 25 release, and inflammation.[21]
Associated with itaconate-regulated functions
[edit]A study reported in 2023 was the first and to date (2024) only study indicating that itaconate's actions are mediated by activating OXGR1. This study showed that itaconate stimulated the nasal secretion of mucus when applied to the noses of mice, reduced the number of Pseudomonas aeruginosa bacteria in their lung tissue and bronchoalveolar lavage fluid (i.e., airway washing) in mice injected intranasally with these bacteria, and stimulated cultured mouse respiratory epithelium cells to raise their cytosolic Ca2+ levels (an indicator of cell activation). Itaconate was unable to induce these responses in OXGR1 gene knockout mice or in the respiratory epithelial cells isolated from the OXGR1 gene knockout mice. The study concluded that the activation of OXGR1 by itaconate contributes to regulating the pulmonary innate immune response to Pseudomonas aeruginosa and might also do so in other bacterial infections.[8][16]
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000165621 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000044819 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c d e f g h i j Kanaoka Y, Maekawa A, Austen KF (April 2013). "Identification of GPR99 protein as a potential third cysteinyl leukotriene receptor with a preference for leukotriene E4 ligand". The Journal of Biological Chemistry. 288 (16): 10967–72. doi:10.1074/jbc.C113.453704. PMC 3630866. PMID 23504326.
- ^ a b c Yamamoto T, Miyata J, Arita M, Fukunaga K, Kawana A (November 2019). "Current state and future prospect of the therapeutic strategy targeting cysteinyl leukotriene metabolism in asthma". Respiratory Investigation. 57 (6): 534–543. doi:10.1016/j.resinv.2019.08.003. PMID 31591069.
- ^ a b Grimm PR, Welling PA (September 2017). "α-Ketoglutarate drives electroneutral NaCl reabsorption in intercalated cells by activating a G-protein coupled receptor, Oxgr1". Current Opinion in Nephrology and Hypertension. 26 (5): 426–433. doi:10.1097/MNH.0000000000000353. PMID 28771454.
- ^ a b c d e f Zeng YR, Song JB, Wang D, Huang ZX, Zhang C, Sun YP, Shu G, Xiong Y, Guan KL, Ye D, Wang P (March 2023). "The immunometabolite itaconate stimulates OXGR1 to promote mucociliary clearance during the pulmonary innate immune response". The Journal of Clinical Investigation. 133 (6). doi:10.1172/JCI160463. PMC 10014103. PMID 36919698.
- ^ a b c d Sasaki F, Yokomizo T (August 2019). "The leukotriene receptors as therapeutic targets of inflammatory diseases". International Immunology. 31 (9): 607–615. doi:10.1093/intimm/dxz044. PMID 31135881.
- ^ Lee DK, Nguyen T, Lynch KR, Cheng R, Vanti WB, Arkhitko O, Lewis T, Evans JF, George SR, O'Dowd BF (2001). "Discovery and mapping of ten novel G protein-coupled receptor genes". Gene. 275 (1): 83–91. doi:10.1016/s0378-1119(01)00651-5. PMID 11574155.
- ^ a b Wittenberger T, Hellebrand S, Munck A, Kreienkamp HJ, Schaller HC, Hampe W (July 2002). "GPR99, a new G protein-coupled receptor with homology to a new subgroup of nucleotide receptors". BMC Genomics. 3: 17. doi:10.1186/1471-2164-3-17. PMC 117779. PMID 12098360.
- ^ Inbe H, Watanabe S, Miyawaki M, Tanabe E, Encinas JA (2004). "Identification and characterization of a cell-surface receptor, P2Y15, for AMP and adenosine". The Journal of Biological Chemistry. 279 (19): 19790–9. doi:10.1074/jbc.M400360200. PMID 15001573.
- ^ Abbracchio MP, Burnstock G, Boeynaems JM, Barnard EA, Boyer JL, Kennedy C, Miras-Portugal MT, King BF, Gachet C, Jacobson KA, Weisman GA (2005). "The recently deorphanized GPR80 (GPR99) proposed to be the P2Y15 receptor is not a genuine P2Y receptor". Trends in Pharmacological Sciences. 26 (1): 8–9. doi:10.1016/j.tips.2004.10.010. PMC 6905457. PMID 15629198.
- ^ He W, Miao FJ, Lin DC, Schwandner RT, Wang Z, Gao J, Chen JL, Tian H, Ling L (May 2004). "Citric acid cycle intermediates as ligands for orphan G-protein-coupled receptors". Nature. 429 (6988): 188–93. Bibcode:2004Natur.429..188H. doi:10.1038/nature02488. PMID 15141213.
- ^ Davenport AP, Alexander SP, Sharman JL, Pawson AJ, Benson HE, Monaghan AE, Liew WC, Mpamhanga CP, Bonner TI, Neubig RR, Pin JP, Spedding M, Harmar AJ (2013). "International Union of Basic and Clinical Pharmacology. LXXXVIII. G protein-coupled receptor list: recommendations for new pairings with cognate ligands". Pharmacological Reviews. 65 (3): 967–86. doi:10.1124/pr.112.007179. PMC 3698937. PMID 23686350.
- ^ a b c Ye D, Wang P, Chen LL, Guan KL, Xiong Y (March 2024). "Itaconate in host inflammation and defense". Trends in Endocrinology and Metabolism. doi:10.1016/j.tem.2024.02.004. PMID 38448252.
- ^ Gonzalez NS, Communi D, Hannedouche S, Boeynaems JM (December 2004). "The fate of P2Y-related orphan receptors: GPR80/99 and GPR91 are receptors of dicarboxylic acids". Purinergic Signalling. 1 (1): 17–20. doi:10.1007/s11302-004-5071-6. PMC 2096567. PMID 18404396.
- ^ "Oxoglutarate receptor | Oxoglutarate receptor | IUPHAR/BPS Guide to PHARMACOLOGY".
- ^ Bäck M, Powell WS, Dahlén SE, Drazen JM, Evans JF, Serhan CN, Shimizu T, Yokomizo T, Rovati GE (2014). "Update on leukotriene, lipoxin and oxoeicosanoid receptors: IUPHAR Review 7". British Journal of Pharmacology. 171 (15): 3551–74. doi:10.1111/bph.12665. PMC 4128057. PMID 24588652.
- ^ Maekawa A, Kanaoka Y, Xing W, Austen KF (October 2008). "Functional recognition of a distinct receptor preferential for leukotriene E4 in mice lacking the cysteinyl leukotriene 1 and 2 receptors". Proceedings of the National Academy of Sciences of the United States of America. 105 (43): 16695–700. doi:10.1073/pnas.0808993105. PMC 2575482. PMID 18931305.
- ^ a b Bankova LG, Dwyer DF, Yoshimoto E, Ualiyeva S, McGinty JW, Raff H, von Moltke J, Kanaoka Y, Frank Austen K, Barrett NA (October 2018). "The cysteinyl leukotriene 3 receptor regulates expansion of IL-25-producing airway brush cells leading to type 2 inflammation". Science Immunology. 3 (28). doi:10.1126/sciimmunol.aat9453. PMC 6599626. PMID 30291131.
- ^ a b Foster HR, Fuerst E, Branchett W, Lee TH, Cousins DJ, Woszczek G (February 2016). "Leukotriene E4 is a full functional agonist for human cysteinyl leukotriene type 1 receptor-dependent gene expression". Scientific Reports. 6: 20461. doi:10.1038/srep20461. PMC 4735867. PMID 26830450.
- ^ Parmentier CN, Fuerst E, McDonald J, Bowen H, Lee TH, Pease JE, Woszczek G, Cousins DJ (April 2012). "Human T(H)2 cells respond to cysteinyl leukotrienes through selective expression of cysteinyl leukotriene receptor 1". The Journal of Allergy and Clinical Immunology. 129 (4): 1136–42. doi:10.1016/j.jaci.2012.01.057. PMID 22391114.
- ^ Doherty TA, Khorram N, Lund S, Mehta AK, Croft M, Broide DH (July 2013). "Lung type 2 innate lymphoid cells express cysteinyl leukotriene receptor 1, which regulates TH2 cytokine production". The Journal of Allergy and Clinical Immunology. 132 (1): 205–13. doi:10.1016/j.jaci.2013.03.048. PMC 3704056. PMID 23688412.
- ^ a b Pu S, Zhang J, Ren C, Zhou H, Wang Y, Wu Y, Yang S, Cao F, Zhou H (July 2023). "Montelukast prevents mice against carbon tetrachloride- and methionine-choline deficient diet-induced liver fibrosis: Reducing hepatic stellate cell activation and inflammation". Life Sciences. 325: 121772. doi:10.1016/j.lfs.2023.121772. PMID 37178864.
- ^ Guerrero A, Visniauskas B, Cárdenas P, Figueroa SM, Vivanco J, Salinas-Parra N, Araos P, Nguyen QM, Kassan M, Amador CA, Prieto MC, Gonzalez AA (2021). "α-Ketoglutarate Upregulates Collecting Duct (Pro)renin Receptor Expression, Tubular Angiotensin II Formation, and Na+ Reabsorption During High Glucose Conditions". Frontiers in Cardiovascular Medicine. 8: 644797. doi:10.3389/fcvm.2021.644797. PMC 8220822. PMID 34179130.
- ^ Steinke JW, Negri J, Payne SC, Borish L (2014). "Biological effects of leukotriene E4 on eosinophils". Prostaglandins, Leukotrienes, and Essential Fatty Acids. 91 (3): 105–10. doi:10.1016/j.plefa.2014.02.006. PMC 4127125. PMID 24768603.
- ^ Shirasaki H, Kanaizumi E, Himi T (2016). "Expression and localization of OXGR1 in human nasal mucosa". Auris, Nasus, Larynx. 44 (2): 162–167. doi:10.1016/j.anl.2016.05.010. PMID 27324180.
- ^ a b c Bankova LG, Lai J, Yoshimoto E, Boyce JA, Austen KF, Kanaoka Y, Barrett NA (May 2016). "Leukotriene E4 elicits respiratory epithelial cell mucin release through the G-protein-coupled receptor, GPR99". Proceedings of the National Academy of Sciences of the United States of America. 113 (22): 6242–7. doi:10.1073/pnas.1605957113. PMC 4896673. PMID 27185938.
- ^ Mittal R, Parrish JM, Soni M, Mittal J, Mathee K (October 2018). "Microbial otitis media: recent advancements in treatment, current challenges and opportunities". Journal of Medical Microbiology. 67 (10): 1417–1425. doi:10.1099/jmm.0.000810. PMID 30084766.
- ^ Kerschner JE, Hong W, Taylor SR, Kerschner JA, Khampang P, Wrege KC, North PE (2013). "A novel model of spontaneous otitis media with effusion (OME) in the Oxgr1 knock-out mouse". International Journal of Pediatric Otorhinolaryngology. 77 (1): 79–84. doi:10.1016/j.ijporl.2012.09.037. PMC 3535456. PMID 23200873.
- ^ Majmundar AJ, Widmeier E, Heneghan JF, Daga A, Wu CW, Buerger F, Hugo H, Ullah I, Amar A, Ottlewski I, Braun DA, Jobst-Schwan T, Lawson JA, Zahoor MY, Rodig NM, Tasic V, Nelson CP, Khaliq S, Schönauer R, Halbritter J, Sayer JA, Fathy HM, Baum MA, Shril S, Mane S, Alper SL, Hildebrandt F (March 2023). "OXGR1 is a candidate disease gene for human calcium oxalate nephrolithiasis". Genetics in Medicine. 25 (3): 100351. doi:10.1016/j.gim.2022.11.019. PMC 9992313. PMID 36571463.
- ^ Tokonami N, Morla L, Centeno G, Mordasini D, Ramakrishnan SK, Nikolaeva S, Wagner CA, Bonny O, Houillier P, Doucet A, Firsov D (July 2013). "α-Ketoglutarate regulates acid-base balance through an intrarenal paracrine mechanism". The Journal of Clinical Investigation. 123 (7): 3166–71. doi:10.1172/JCI67562. PMC 3696567. PMID 23934124.
- ^ Yuan Y, Zhu C, Wang Y, Sun J, Feng J, Ma Z, Li P, Peng W, Yin C, Xu G, Xu P, Jiang Y, Jiang Q, Shu G (May 2022). "α-Ketoglutaric acid ameliorates hyperglycemia in diabetes by inhibiting hepatic gluconeogenesis via serpina1e signaling". Science Advances. 8 (18): eabn2879. Bibcode:2022SciA....8N2879Y. doi:10.1126/sciadv.abn2879. PMC 9067931. PMID 35507647.
- ^ a b Yuan Y, Xu P, Jiang Q, Cai X, Wang T, Peng W, Sun J, Zhu C, Zhang C, Yue D, He Z, Yang J, Zeng Y, Du M, Zhang F, Ibrahimi L, Schaul S, Jiang Y, Wang J, Sun J, Wang Q, Liu L, Wang S, Wang L, Zhu X, Gao P, Xi Q, Yin C, Li F, Xu G, Zhang Y, Shu G (April 2020). "Exercise-induced α-ketoglutaric acid stimulates muscle hypertrophy and fat loss through OXGR1-dependent adrenal activation". The EMBO Journal. 39 (7): e103304. doi:10.15252/embj.2019103304. PMC 7110140. PMID 32104923.
- ^ Sánchez P, Vélez-Del-Burgo A, Suñén E, Martínez J, Postigo I (March 2022). "Fungal Allergen and Mold Allergy Diagnosis: Role and Relevance of Alternaria alternata Alt a 1 Protein Family". Journal of Fungi. 8 (3): 277. doi:10.3390/jof8030277. PMC 8954643. PMID 35330279.
- ^ Ualiyeva S, Hallen N, Kanaoka Y, Ledderose C, Matsumoto I, Junger WG, Barrett NA, Bankova LG (January 2020). "Airway brush cells generate cysteinyl leukotrienes through the ATP sensor P2Y2". Science Immunology. 5 (43). doi:10.1126/sciimmunol.aax7224. PMC 7176051. PMID 31953256.
Further reading
[edit]- Lee DK, Nguyen T, Lynch KR, Cheng R, Vanti WB, Arkhitko O, Lewis T, Evans JF, George SR, O'Dowd BF (Sep 2001). "Discovery and mapping of ten novel G protein-coupled receptor genes". Gene. 275 (1): 83–91. doi:10.1016/S0378-1119(01)00651-5. PMID 11574155.
- Takeda S, Kadowaki S, Haga T, Takaesu H, Mitaku S (Jun 2002). "Identification of G protein-coupled receptor genes from the human genome sequence". FEBS Letters. 520 (1–3): 97–101. Bibcode:2002FEBSL.520...97T. doi:10.1016/S0014-5793(02)02775-8. PMID 12044878.
- Inbe H, Watanabe S, Miyawaki M, Tanabe E, Encinas JA (May 2004). "Identification and characterization of a cell-surface receptor, P2Y15, for AMP and adenosine". The Journal of Biological Chemistry. 279 (19): 19790–9. doi:10.1074/jbc.M400360200. PMID 15001573.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.